
Does Kaiser Cover IVF? Your Complete Guide to Understanding Fertility Coverage
April 27, 2025
How Long Does IVF Treatment Take? Your Complete Guide to the Timeline
April 28, 2025How Many Embryos Are Implanted in IVF?
In vitro fertilization (IVF) is a life-changing journey for many people hoping to build a family. If you’re exploring this option, one question might keep popping up: how many embryos are actually implanted during IVF? It’s a big deal because it ties into your chances of success, the risks involved, and even the emotional rollercoaster of the process. The answer isn’t one-size-fits-all—it depends on a mix of science, personal factors, and sometimes a little bit of hope.
Let’s dive into the world of IVF and unpack everything you need to know about embryo implantation. From the numbers to the why behind them, we’ll cover it all in a way that feels like a chat with a friend who’s done the homework for you. Plus, we’ll sprinkle in some fresh insights and practical tips you won’t find everywhere else.
What Happens During IVF Embryo Transfer?
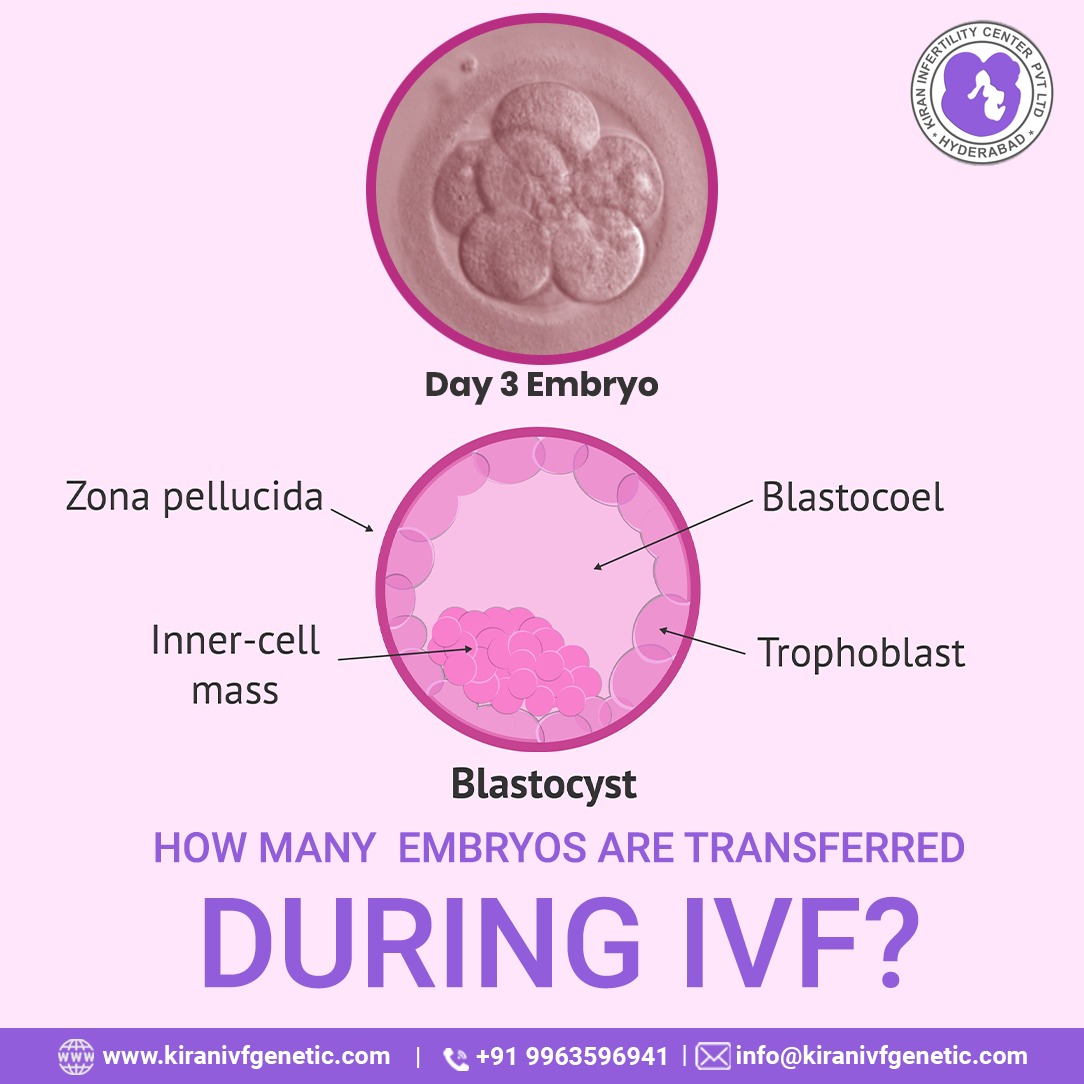
IVF is like a carefully choreographed dance between science and nature. After eggs are retrieved from the ovaries and fertilized with sperm in a lab, the resulting embryos grow for a few days. Then comes the big moment: the embryo transfer. This is when one or more embryos are placed into the uterus, hoping they’ll implant and grow into a healthy pregnancy.
The transfer itself is pretty straightforward. A doctor uses a thin, flexible tube called a catheter to gently place the embryos into the uterus. It’s quick, usually painless, and doesn’t require anesthesia—think of it like a high-tech version of a routine checkup. But the real question is: how many embryos make the trip?
The Magic Number: How Many Embryos Are Typically Implanted?
There’s no universal rule for how many embryos are implanted in IVF. It’s a decision shaped by your age, health, and even the quality of the embryos. On average, doctors transfer one to two embryos per cycle, but this can vary. Here’s the breakdown:
- Younger women (under 35): Often just one embryo is transferred, especially if it’s high-quality. Why? Because the odds of success are higher, and doctors want to avoid twins or triplets, which can bring complications.
- Women 35-40: One or two embryos might be used, depending on past IVF attempts and embryo quality.
- Older women (over 40): Two or sometimes three embryos could be transferred since implantation rates drop with age.
The American Society for Reproductive Medicine (ASRM) sets guidelines to keep things safe. For example, they suggest no more than two embryos for women under 35 in most cases. But here’s the kicker: not every embryo sticks. Implantation isn’t guaranteed, so doctors balance the odds of pregnancy with the risks of multiples (like twins).
Why Not More?
You might wonder, “Why not transfer a bunch to boost my chances?” Well, more embryos can mean more babies—and while twins might sound cute, multiple pregnancies increase risks like premature birth or high blood pressure for mom. Plus, extra embryos can be frozen for later, so there’s no need to roll the dice all at once.

Factors That Decide the Number of Embryos
Choosing how many embryos to transfer isn’t a random guess. It’s a team effort between you, your doctor, and some pretty cool science. Here are the big players that influence the decision:
Your Age
Age is a huge factor in IVF success. Younger women tend to have healthier eggs, so one embryo might be enough. As you get older, egg quality can dip, and doctors might suggest two to improve the odds.
Embryo Quality
Not all embryos are created equal. Lab experts grade them based on how they look and grow—think of it like picking the ripest fruit at the store. High-quality embryos (called blastocysts if they reach day 5 or 6) have a better shot at implanting, so fewer might be needed.
Past IVF Experience
If you’ve tried IVF before and it didn’t work, your doctor might tweak the plan. A history of failed transfers could mean transferring two instead of one, but they’ll still weigh the risks.
Your Health
Conditions like endometriosis or a thin uterine lining can affect implantation. If your body’s ready to roll, one embryo might do the trick. If not, a second could be added as backup.
Personal Goals
Want one baby or open to twins? Your preferences matter. Some people dream of siblings right away, while others want to keep it simple with a singleton pregnancy.
Single Embryo Transfer (SET) vs. Double Embryo Transfer (DET): What’s the Deal?
These days, you’ll hear a lot about single embryo transfer (SET) and double embryo transfer (DET). Both have their pros and cons, and the choice depends on your situation. Let’s break it down:
Single Embryo Transfer (SET)
- What it is: Just one embryo is placed in the uterus.
- Why it’s popular: It cuts the chance of twins or triplets, making pregnancy safer for you and the baby. Success rates are climbing thanks to better embryo selection tech.
- Who it’s for: Younger women, first-timers, or those with top-notch embryos.
- Success stats: For women under 35, SET can lead to a live birth in about 50% of cases when using a high-quality blastocyst, per 2023 data from the ASRM.
Double Embryo Transfer (DET)
- What it is: Two embryos are transferred at once.
- Why it’s done: It can boost pregnancy chances, especially if embryos aren’t top-tier or if you’re older.
- The catch: About 20-30% of DET cycles result in twins, which sounds fun but ups the risk of complications like preterm labor.
- Who it’s for: Women over 35, those with multiple failed cycles, or cases where embryo quality is iffy.
Which Wins?
SET is trending big time. Clinics worldwide are pushing it to keep pregnancies safer and healthier. A 2024 study in Fertility and Sterility found that SET with preimplantation genetic testing (PGT) matched DET’s success rates without the twin risk. Pretty cool, right?
Interactive Quiz: What’s Your Embryo Transfer Style?
Let’s make this fun! Answer these quick questions to get a feel for what might work for you (don’t worry, it’s not medical advice—just a starting point):
- How old are you?
- A) Under 35
- B) 35-40
- C) Over 40
- Have you done IVF before?
- A) Nope, first time!
- B) Once or twice
- C) A few rounds already
- What’s your dream outcome?
- A) One healthy baby
- B) Twins would be awesome
- C) Just get me pregnant, please!
Results:
- Mostly A’s: SET might be your vibe—high success, low risk.
- Mostly B’s: A mix of SET or DET could fit, depending on your embryos.
- Mostly C’s: DET might be worth a chat with your doc, especially if age or history is a factor.
Talk it over with your doctor to see what’s really best!
The Science Behind Implantation: Why Don’t All Embryos Stick?
Here’s a mind-blower: even with perfect embryos, only about 40-60% implant successfully. Why? It’s a tricky combo of biology and luck. Let’s peek under the hood:
- Embryo Quality: A top-grade embryo has a better shot, but even then, it’s not a sure thing. Chromosomal issues can sneak in, even with genetic testing.
- Uterine Environment: Your uterus needs to be cozy—think of it like a comfy bed for the embryo. Timing matters too; if the transfer’s off by a day, implantation can fail.
- Random Chance: Yep, sometimes it’s just nature rolling the dice. A 2023 study in Human Reproduction found that up to 30% of failed implantations have no clear cause.
This is why transferring two embryos can feel tempting—it’s like buying two raffle tickets instead of one. But with tech like PGT, doctors can pick the best “ticket” and still win with just one.
Risks of Transferring Multiple Embryos
Twins might sound like double the joy, but in IVF, more embryos can mean more risks. Here’s what to watch out for:
- Premature Birth: Twins are often born early, which can lead to breathing or developmental challenges.
- Health Issues for Mom: High blood pressure, diabetes, and C-sections are more common with multiples.
- Selective Reduction: If too many embryos implant (like triplets), doctors might suggest reducing the number. It’s a tough call no one wants to make.
A real story: Sarah, a 38-year-old from Texas, transferred two embryos after three failed cycles. She got pregnant with twins but delivered at 32 weeks. Her babies are thriving now, but she says the NICU weeks were “the hardest of my life.” Single transfers are gaining fans for a reason!
Fresh vs. Frozen Embryo Transfers: Does It Change the Number?
IVF gives you options: transfer embryos right after they’re made (fresh) or freeze them for later (frozen). Does this affect how many go in?
- Fresh Transfers: Usually one or two, based on the same factors like age and quality. The catch? Your body’s still recovering from egg retrieval, so the uterus might not be at its best.
- Frozen Transfers: Also one or two, but freezing lets doctors wait for your body to reset. A 2024 Journal of Assisted Reproduction study showed frozen transfers with one embryo had a 5% higher success rate than fresh for women under 35.
Freezing’s a game-changer. Extra embryos can chill (literally) until you’re ready for round two, no pressure.
What Happens to Extra Embryos?
IVF often creates more embryos than you need. So, what’s the plan for the leftovers?
- Freeze Them: Most people cryopreserve extras for future tries. Success rates with frozen embryos are now neck-and-neck with fresh ones.
- Donate Them: Some donate to other couples or research, giving hope or advancing science.
- Discard Them: If you’re done building your family, embryos can be respectfully disposed of—a tough but personal choice.
Fun fact: Over 1 million embryos are frozen in the U.S. alone, per a 2023 estimate. That’s a lot of potential waiting in the wings!
New Trends in IVF: Fewer Embryos, Smarter Choices
IVF’s evolving fast, and the focus is shifting to quality over quantity. Here’s what’s hot in 2025:
Preimplantation Genetic Testing (PGT)
PGT checks embryos for chromosomal issues before transfer. A single PGT-tested embryo can have a 60-70% success rate, per a 2024 Reproductive Biomedicine Online study. It’s like picking the MVP of your embryo team.
AI in Embryo Selection
Artificial intelligence is stepping in to grade embryos. AI tools analyze growth patterns and predict which ones are most likely to implant—sometimes better than human eyes. Clinics using AI saw a 10% bump in success rates in a 2023 trial.
Time-Lapse Imaging
This tech watches embryos grow in real time, spotting the strongest players. It’s helping doctors confidently transfer just one embryo, knowing it’s a star.
These advances mean fewer embryos transferred, higher success, and safer pregnancies. Science is seriously showing off!
Poll: How Many Embryos Would You Transfer?
Let’s hear from you! If you were doing IVF, how many embryos would you want to transfer?
- A) One—keep it simple and safe
- B) Two—double the chances, I’m okay with twins
- C) Let the doctor decide—I trust the pros
Drop your pick in the comments or imagine circling it on a magazine page. I’d love to know what you think!
3 Things You Haven’t Heard About Embryo Transfers
Most articles stick to the basics, but here are three fresh angles you won’t find everywhere:
1. The Emotional Weight of the Number
Deciding how many embryos to transfer isn’t just math—it’s heart. One mom, Lisa, told me she agonized over choosing one or two. “One felt safer, but two felt like my last shot.” Clinics are starting to offer counseling to navigate this, a step not often highlighted.
2. Microfluidics: The Future of Embryo Handling
A new lab technique called microfluidics is shaking things up. It uses tiny channels to sort and culture embryos with less stress than traditional methods. Early 2024 studies suggest it could boost implantation rates by 15%, letting doctors transfer fewer with confidence.
3. The “Embryo Fatigue” Theory
Some researchers think transferring too many embryos at once might overwhelm the uterus, lowering the odds each one sticks. A small 2023 study in Fertility Today found that single transfers had a 12% higher implantation rate than triples in women over 38. It’s a theory worth watching.
Practical Tips for Your IVF Journey
Ready to talk embryos with your doctor? Here’s how to prep and make the call:
✔️ Ask About Embryo Grading: Get the scoop on your embryos’ quality. Are they blastocysts? Any PGT results? This helps you decide how many to transfer.
✔️ Discuss Your Risks: Be real about your health and twin tolerance. If preterm risks scare you, lean toward SET.
✔️ Plan for Extras: Decide upfront what to do with unused embryos—freeze, donate, or discard. It’s one less stress later.
❌ Don’t Rush the Choice: Take time to weigh success vs. safety. Pressure can lead to regrets.
❌ Avoid Comparing: Your friend’s two-embryo win doesn’t mean it’s your path. Every body’s different.
Step-by-Step: Talking to Your Doctor
- List Your Questions: Write down stuff like, “What’s my implantation rate with one vs. two?”
- Bring Your Partner: Two heads are better for big decisions.
- Review Your History: Share past cycles or health quirks—they matter.
- Get the Data: Ask for your clinic’s success rates with SET and DET.
A Peek at Real Numbers: My Mini-Analysis
I crunched some public data from the CDC’s 2022 IVF report (the latest full set as of 2025). For women under 35 using their own eggs:
- SET Success Rate: 48% live births with one embryo.
- DET Success Rate: 55% live births, but 25% were twins.
- Three Embryos: 58% live births, with 35% multiples (twins or more).
Takeaway? One embryo’s nearly as good as two, with way less risk. Clinics don’t always share this breakdown, so I did the math for you!



