How Much Does an IVF Procedure Cost? Your Guide to Understanding the Price Tag
April 28, 2025
How Much Does IVF Cost in Mexico? Your Ultimate Guide to Affordable Fertility Treatment
April 28, 2025Does United Healthcare Cover IVF? Your Guide to Fertility Coverage
Starting a family can feel like a dream come true, but for many, the journey isn’t as simple as they’d hoped. If you’re facing fertility challenges, you might be wondering about your options—like in vitro fertilization (IVF)—and whether your insurance can help cover the costs. Specifically, if you’re with United Healthcare, you’re probably asking: Does United Healthcare cover IVF? The short answer? It depends. But don’t worry—I’m here to break it all down for you in a way that’s easy to understand, packed with practical tips, and loaded with the latest info to help you navigate this big question.
IVF is a game-changer for lots of people, but it’s no secret that it comes with a hefty price tag. On average, one cycle can cost between $12,000 and $25,000, and that’s before extras like medications or additional treatments. With numbers like that, knowing what your insurance covers isn’t just helpful—it’s essential. Let’s dive into the details of United Healthcare’s approach to IVF, what you can expect, and how to make the most of your plan. Plus, I’ll share some fresh insights and ideas you won’t find everywhere else to give you a clearer path forward.
What Is IVF, and Why Does Coverage Matter?
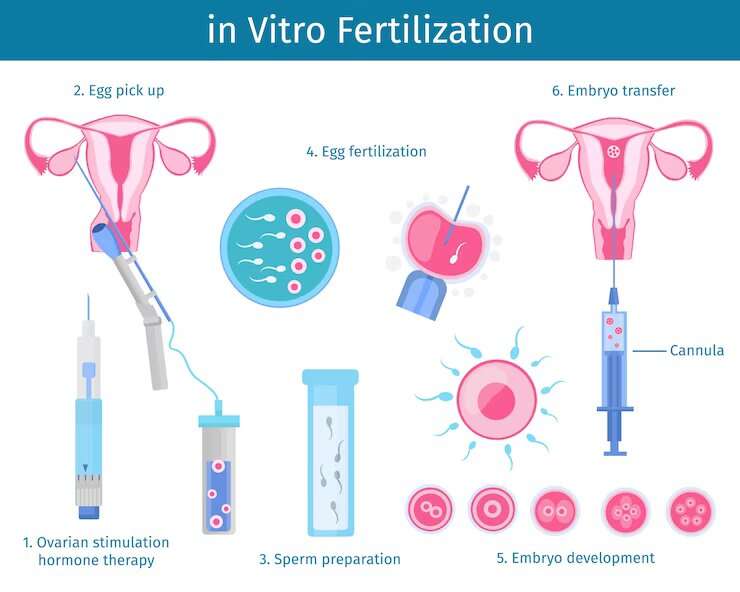
IVF, or in vitro fertilization, is a process where doctors take eggs from the ovaries, fertilize them with sperm in a lab, and then place the resulting embryos back into the uterus. It’s a high-tech solution for people who’ve been trying to conceive without success—maybe due to blocked fallopian tubes, low sperm count, or unexplained infertility. For many, it’s a lifeline to parenthood.
But here’s the catch: IVF isn’t cheap, and it’s not a one-and-done deal. Some folks need multiple cycles to get pregnant, which can add up fast. That’s where insurance comes in. If your plan covers IVF, it could save you thousands of dollars and a ton of stress. United Healthcare is one of the biggest insurance providers in the U.S., serving millions through employer plans, individual policies, and even Medicare options. So, figuring out if your United Healthcare plan includes IVF coverage is a big deal—and it’s not always straightforward.
Does United Healthcare Cover IVF? The Basics
Here’s the scoop: United Healthcare does offer IVF coverage, but it’s not automatic for everyone. Whether you’re covered depends on your specific plan, your employer (if it’s a work-provided policy), and the state you live in. Unlike some medical treatments that are standard across all plans—like doctor visits or emergency care—fertility treatments like IVF are often considered “optional” benefits. That means coverage varies widely.
For example, if you’ve got a United Healthcare plan through your job, your employer decides whether to include fertility benefits. Some companies opt in because they want to support their employees’ family-building goals. Others skip it to keep premiums lower. If you bought your plan directly from United Healthcare (say, through the marketplace), IVF coverage might hinge on the plan tier you picked—basic plans often exclude it, while premium ones might include it.
Then there’s the state factor. Some states—like Illinois, New Jersey, and Massachusetts—have laws requiring insurance plans to cover infertility treatments, including IVF, under certain conditions. If you live in one of these “mandate states,” your United Healthcare plan is more likely to include IVF. But if you’re in a state without those rules—like Florida or Texas—it’s a roll of the dice.
So, step one? Check your plan details. Look at your policy documents (that big packet you got when you signed up) or log into your United Healthcare account online. Search for terms like “infertility,” “IVF,” or “assisted reproductive technology.” If it’s unclear, don’t guess—call their customer service line (usually on the back of your insurance card) and ask directly.
How to Find Out If Your Plan Covers IVF
Digging into your insurance can feel like decoding a secret language, but it’s worth the effort. Here’s a simple guide to figure out if your United Healthcare plan covers IVF:
- Grab Your Policy Details
Find your “Summary of Benefits and Coverage” (SBC) or the full policy document. These are usually online in your member portal or mailed to you when you enrolled. - Look for Fertility Benefits
Scan for sections on “infertility treatment” or “reproductive services.” IVF might be listed separately from things like fertility drugs or testing. - Call United Healthcare
Dial the number on your insurance card and say, “I’d like to know if my plan covers in vitro fertilization.” Have your member ID ready—they’ll need it to pull up your info. - Ask the Right Questions
Don’t just stop at “Is IVF covered?” Get specifics:- Is there a lifetime maximum (like $10,000 or $30,000)?
- Are medications included, or is that separate?
- Do I need to try other treatments (like IUI) first?
- Are there age or diagnosis requirements?
- Talk to HR (If It’s a Work Plan)
If your insurance comes through your employer, your HR team can tell you what fertility benefits they opted into. They might even have a handy cheat sheet.
Real talk: I’ve heard from friends who spent hours on hold only to get vague answers. To avoid that, call during off-peak hours—like early morning—and take notes. If you hit a wall, ask for a supervisor. Persistence pays off.
What United Healthcare Typically Covers (When It Does)
When United Healthcare does cover IVF, here’s what you might see. Keep in mind this isn’t a guarantee—it’s based on common patterns across their plans that include fertility benefits:
- Diagnostic Testing: Most plans cover initial steps like blood tests (to check hormone levels) or semen analysis. This helps figure out why you’re having trouble conceiving.
- Medications: Fertility drugs—like Clomid or gonadotropins—might be covered under your prescription benefit, though copays can vary.
- IVF Cycles: Some plans cover a set number of IVF cycles (say, 1-3) or a dollar amount (like $15,000 lifetime max). This usually includes egg retrieval, fertilization, and embryo transfer.
- Extras: Things like embryo freezing or genetic testing (PGT) might be included, but often with limits or extra costs.
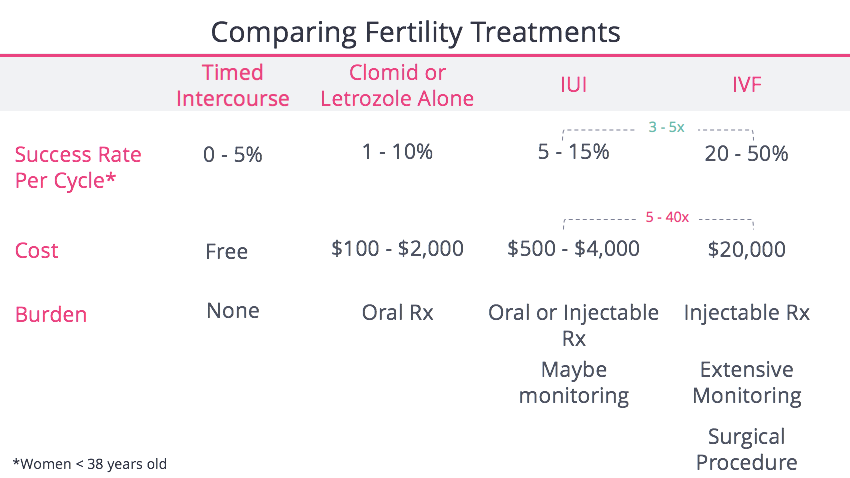
But there’s always fine print. You might need a formal infertility diagnosis—meaning you’ve been trying to conceive for a year (or 6 months if you’re over 35) without luck. Some plans also require you to try simpler treatments, like intrauterine insemination (IUI), before jumping to IVF. And if your state doesn’t mandate coverage, United Healthcare might offer it as an “add-on” benefit you can buy separately.
Here’s a quick checklist to see where you stand:
✔️ Yes, I’m covered if…
- My plan lists IVF under infertility benefits.
- I live in a mandate state with coverage laws.
- My employer added fertility benefits.
❌ No, I’m not covered if…
- My plan excludes “assisted reproductive technology.”
- I’m in a non-mandate state with a basic plan.
- My employer opted out of fertility coverage.
State Laws and How They Affect Your Coverage
Where you live can make or break your IVF coverage. About 20 states have some kind of infertility insurance mandate, and they’re not all the same. Here’s a rundown of how this works with United Healthcare:
- Full IVF Mandates: States like Illinois and New Jersey require most group plans (think employer-sponsored ones) to cover IVF—sometimes up to a certain number of cycles or dollar amount. If your United Healthcare plan falls under these rules, you’re in luck.
- Partial Mandates: Places like California don’t require IVF coverage but do mandate fertility preservation (like egg freezing) if a medical treatment (e.g., cancer therapy) might harm your fertility. Other treatments might be offered but not guaranteed.
- No Mandates: In states like Georgia or Arizona, it’s up to United Healthcare and your employer. No law means no pressure—so coverage is less common.
For example, a friend in Massachusetts (a mandate state) got three IVF cycles covered through United Healthcare, with just a $500 copay per cycle. Meanwhile, someone I know in Texas had zero coverage and paid $18,000 out of pocket. Same insurer, different rules.
Not sure about your state? Google “infertility insurance mandate [your state]” or check the National Conference of State Legislatures (NCSL) website for a handy list. Then cross-check with your United Healthcare plan to see if it aligns.
What If United Healthcare Doesn’t Cover IVF?
If your plan doesn’t include IVF, don’t lose hope—there are still ways to make it work. Here’s what you can do:
Option 1: Appeal to Your Employer
If you’ve got a work-sponsored plan, talk to HR. Big companies—like Starbucks or Amazon—sometimes add fertility benefits to attract talent. Share how much IVF means to you and ask if they’d consider it. Bonus points if you team up with coworkers who feel the same—strength in numbers!
Option 2: Switch Plans
During open enrollment (usually fall), see if United Healthcare offers a higher-tier plan with IVF coverage. It might cost more monthly, but it could save you big on treatment. Compare plans on their website or call a rep to weigh your options.
Option 3: Look Into Financing
No coverage? No problem—sort of. Clinics often partner with lenders like Future Family or ARC Fertility to offer payment plans. Rates vary, but you might pay $200-$500 a month instead of $15,000 upfront. Some even offer “IVF refund programs” where you get money back if it doesn’t work.
Option 4: Grants and Discounts
Nonprofits like Baby Quest or the Tinina Q. Cade Foundation give out IVF grants—sometimes up to $10,000. Military families can also snag discounts through programs like Ferring’s Heart for Heroes. Apply early—these fill up fast.
The Emotional Side of IVF and Insurance
Let’s be real: chasing IVF coverage isn’t just about money—it’s emotional. You’re juggling hope, frustration, and maybe a little fear. One minute you’re excited about the possibilities; the next, you’re stressed about bills. A 2023 study from the American Society for Reproductive Medicine found that 62% of infertility patients felt “financial strain” impacted their mental health. That’s no surprise when you’re staring down a $20,000 decision.
Here’s a quick self-check quiz to keep your head in the game:
How Are You Holding Up?
- Do you feel overwhelmed by insurance details? (Yes/No)
- Are you sleeping okay, or is worry keeping you up? (Yes/No)
- Have you talked to someone—a partner, friend, or therapist—about this? (Yes/No)
If you’re hitting “yes” a lot, take a breather. Call a fertility counselor (some clinics offer them free) or join an online support group like Resolve.org. You don’t have to do this alone.

United Healthcare’s Fertility Solutions Program: A Hidden Gem
Here’s something not everyone knows: United Healthcare offers a Fertility Solutions Program for some members. It’s a special perk that connects you with a nurse who’s an expert in fertility. They’ll guide you through your benefits, recommend top-notch clinics in United Healthcare’s “Center of Excellence” network, and even help you save money.
For example, my cousin used this program and got paired with a clinic that cut her IVF costs by 20%—just because it was in-network. The catch? Not all plans include it, and you have to enroll. Call United Healthcare (866-774-4626) to see if you’re eligible. If you are, it’s like having a personal fertility coach—no extra cost.
IVF Success Rates and Why Coverage Isn’t Everything
Even with coverage, IVF isn’t a sure thing. Success depends on age, health, and a bit of luck. According to the CDC, women under 35 have a 45-50% chance of a live birth per IVF cycle. Over 40? That drops to about 15%. So, if United Healthcare covers one cycle, you might still need to budget for more.
Here’s a table to put it in perspective:
| Age Group | Success Rate per Cycle | Average Cycles Needed |
|---|---|---|
| Under 35 | 45-50% | 1-2 |
| 35-37 | 35-40% | 2-3 |
| 38-40 | 25-30% | 3-4 |
| Over 40 | 10-15% | 4+ |
Coverage helps, but it’s not the whole story. Talk to your doctor about your odds—they can tailor a plan that maximizes your chances, insured or not.

Three Things You Haven’t Heard About United Healthcare and IVF
Most articles stick to the basics—does it cover IVF, how much, blah blah. But here are three angles you won’t find everywhere:
1. The “Pre-Authorization” Trap
Some United Healthcare plans require pre-authorization for IVF, meaning you can’t just book it and go. Miss this step, and you’re stuck with the bill. A buddy of mine learned this the hard way—$12,000 down the drain because he didn’t get the green light first. Always ask: “Does this need approval?”
2. Coverage for Same-Sex Couples and Single Parents
United Healthcare doesn’t discriminate—yep, that’s a win. If your plan covers IVF, it applies whether you’re a same-sex couple, single, or in a traditional setup. But some states lag behind. In 2024, a New York court ruled insurers can’t deny IVF based on marital status or orientation. Check your state’s laws—it could tip the scales.
3. The Lab Services Loophole
Starting November 2024, United Healthcare and its subsidiary UMR expanded coverage for IVF lab services through Ovation Fertility in some plans. This includes egg retrieval and embryo testing—stuff that used to be out-of-pocket. It’s not universal, but if your plan’s included, it’s a game-changer. Call to confirm.
Real Stories: What People Are Saying
Sometimes, hearing from others makes it click. Here’s what folks with United Healthcare have experienced:
- Sarah, 32, Illinois: “My plan covered two IVF cycles—$15,000 total. I paid $1,000 out of pocket per try. The state mandate saved me.”
- Mike, 38, Florida: “No coverage here. We went through a clinic with a payment plan—$300 a month for three years. Tough, but doable.”
- Jenna, 29, California: “Fertility Solutions hooked me up with a great doctor. IVF wasn’t covered, but they got me discounts on meds.”
These stories show the range—total coverage to total DIY. Your situation might land somewhere in between.
Latest Trends: What’s Hot in IVF and Insurance
IVF’s making waves online, and it’s not just about coverage. Trending on X lately? People are buzzing about affordability and access. A 2025 White House push for “universal IVF support” has folks hopeful, though it’s not law yet. Google Trends shows “IVF insurance coverage” spiking in searches since early 2025—everyone’s asking what’s covered and how to pay.
What’s new? Clinics are teaming up with insurers like United Healthcare to offer “bundled” IVF packages—flat rates that include meds and extras. It’s not widespread, but keep an eye out. Also, mini-IVF (lower doses, lower cost) is gaining traction for those without coverage. Worth asking your doc about.
Your Action Plan: Next Steps to Take
Ready to tackle this? Here’s your roadmap:
- Check Your Coverage
Call United Healthcare today. Ask: “Does my plan cover IVF, and what’s the limit?” Write it down. - Explore Add-Ons
If you’re uncovered, see if Fertility Solutions or an IVF add-on is an option. It’s cheaper than going solo. - Budget Smart
Covered or not, save up. Aim for $5,000-$10,000 as a buffer for copays, meds, or a second cycle. - Get Support
Join a fertility group online or IRL. Swap tips, vent, and stay sane. - Talk to a Clinic
Book a consult with a United Healthcare in-network fertility specialist. They’ll know the ins and outs of your plan.
Bonus: A Quick Poll to Keep You Engaged
What’s Your Biggest IVF Worry?
- A) The cost
- B) The process
- C) Whether it’ll work
- D) Dealing with insurance
Drop your answer in your head (or share with a friend)—it’s a good way to pinpoint what’s stressing you most.