Is the Catholic Church Against IVF?
April 24, 2025
What to Do After IVF Transfer: Your Ultimate Guide to Boosting Success
April 25, 2025What IVF Stands For: A Deep Dive into In Vitro Fertilization
In vitro fertilization, or IVF, is a term you might have heard tossed around on TV, in conversations, or maybe even at a family gathering when someone whispers about “fertility stuff.” But what does it actually mean? IVF stands for in vitro fertilization, a process where an egg and sperm meet outside the body—in a lab, to be exact—before being placed back into the uterus to hopefully grow into a baby. It’s like giving nature a little high-tech nudge. If you’re curious about how it works, who it’s for, or what it feels like to go through it, you’re in the right place. This article is your one-stop guide to understanding IVF from top to bottom, with some fresh insights you won’t find everywhere else.
IVF isn’t just a science experiment; it’s a lifeline for millions of people dreaming of starting a family. Over 10 million babies have been born through IVF worldwide since it first burst onto the scene in 1978 with the birth of Louise Brown, the world’s first “test-tube baby.” Today, it’s a household name, but there’s so much more to it than the headlines suggest. Let’s peel back the layers and explore what IVF really stands for—both literally and in the lives of those who experience it.
The Basics of IVF: Breaking It Down
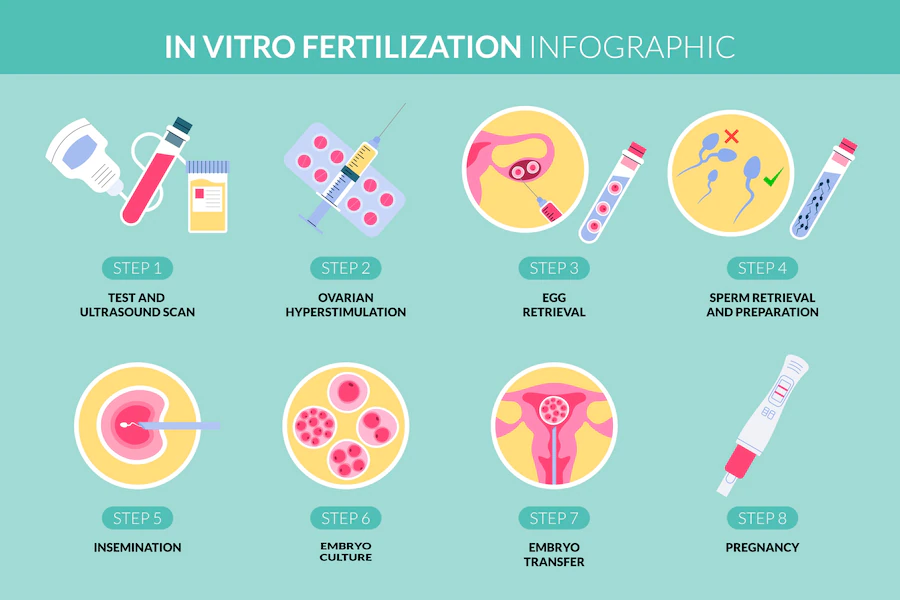
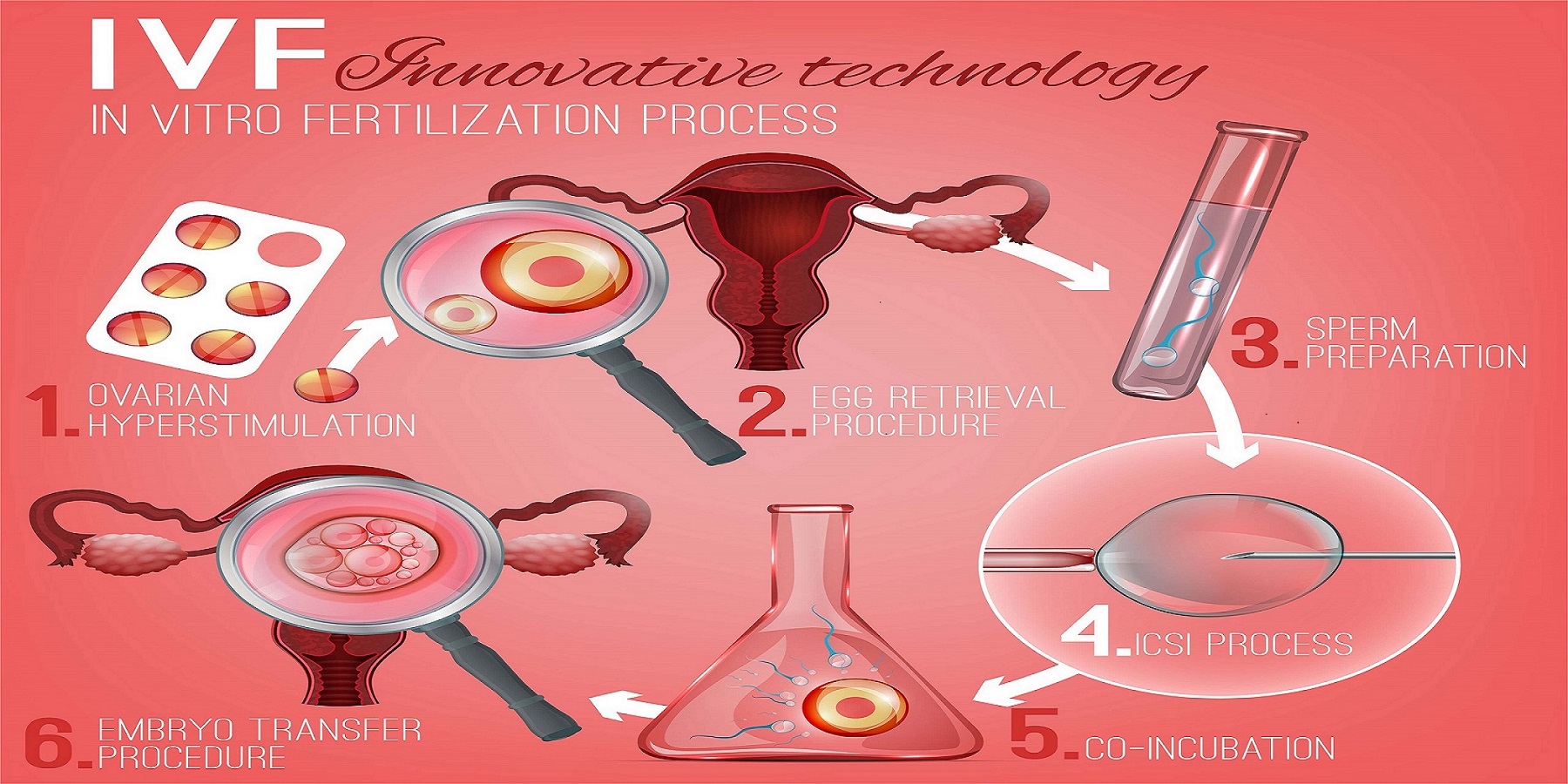
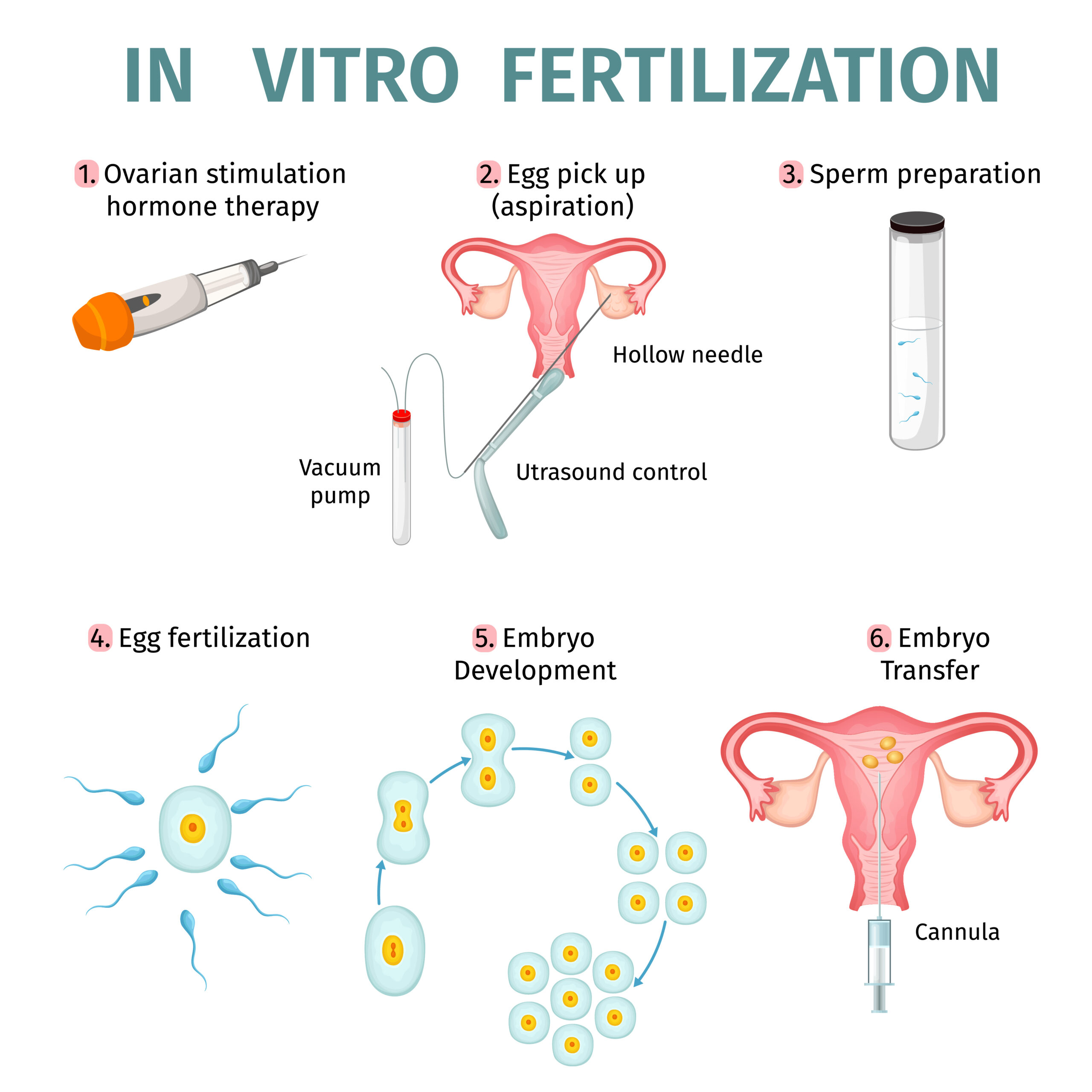
IVF might sound fancy, but at its core, it’s about helping people get pregnant when the usual way isn’t working. The phrase in vitro comes from Latin, meaning “in glass,” because the magic happens in a lab dish, not inside the body. Here’s how it goes in simple terms:
- Egg Boosting: Doctors give the woman medicine to make her ovaries produce more eggs than usual—think of it like revving up an engine.
- Egg Pickup: Those eggs are collected using a tiny needle guided by ultrasound. It’s quick, about 15-30 minutes, and you’re usually asleep for it.
- Sperm Meets Egg: In the lab, the eggs are mixed with sperm (from a partner or donor) to fertilize them. Sometimes, a single sperm is injected into an egg if there’s a sperm quality issue—this is called ICSI (intracytoplasmic sperm injection).
- Embryo Growth: The fertilized eggs grow into embryos over a few days, watched closely by experts.
- Embryo Transfer: One or more embryos are placed into the uterus, hoping they’ll stick and grow into a pregnancy.
That’s the nutshell version! But IVF isn’t one-size-fits-all. Some folks use their own eggs and sperm, while others turn to donors or surrogates. It’s a flexible tool, tailored to each person’s needs.
Who Needs IVF? More People Than You Might Think
IVF isn’t just for one type of person—it’s a solution for all kinds of fertility challenges. About 1 in 6 couples worldwide face infertility, and IVF steps in when other options fall short. Here’s who might turn to it:
- Blocked Fallopian Tubes: If the tubes that carry eggs to the uterus are damaged or blocked, IVF bypasses them entirely.
- Low Sperm Count: When sperm struggles to reach or fertilize an egg, IVF (especially with ICSI) can make it happen.
- Age-Related Issues: As women get older, egg quality drops. IVF can use younger donor eggs or freeze eggs from earlier years.
- Unexplained Infertility: Sometimes, doctors can’t pinpoint why pregnancy isn’t happening—IVF can still help.
- LGBTQ+ Families: Same-sex couples or single folks often use IVF with donors or surrogates to build their families.
Here’s a surprising stat: in 2021, nearly 45% of IVF cycles in women under 35 led to a live birth, according to the Society for Assisted Reproductive Technology. Success rates drop with age, but new tech keeps pushing those numbers up. It’s not a guarantee, but it’s a game-changer for many.
The IVF Journey: What It’s Really Like
Going through IVF is a bit like riding a roller coaster—there are highs, lows, and a whole lot of waiting. Imagine you’re Sarah, a 32-year-old teacher who’s been trying to have a baby for three years. Her doctor suggests IVF, and here’s what her journey might look like:
Step 1: The Prep Phase
Sarah starts with daily hormone shots for about 10-14 days to grow multiple eggs. She feels bloated and moody—side effects that hit about 1 in 5 women, per Yale Medicine. Her partner, Mike, learns to give the shots, turning their kitchen into a mini clinic.
Step 2: Egg Retrieval Day
Under light anesthesia, a doctor collects 12 eggs from Sarah’s ovaries. She’s sore afterward but back to work in a day or two. Meanwhile, Mike provides a sperm sample, which gets prepped in the lab.
Step 3: Waiting for Embryos
Over five days, the lab team watches the embryos grow. Sarah and Mike get a call: eight made it to the blastocyst stage (about 200-300 cells). They’re thrilled but nervous—what if none work?
Step 4: The Transfer
One embryo is placed in Sarah’s uterus using a thin tube. It’s quick and painless, like a Pap smear. Two weeks later, a blood test shows she’s pregnant. They celebrate, but the anxiety lingers until that first ultrasound.
This is just one story. Some need multiple rounds; others face setbacks. The emotional toll is real—studies show up to 40% of IVF patients experience anxiety or depression. Support groups and counseling can make a huge difference.
IVF Success Rates: What the Numbers Say
How likely is IVF to work? It depends on a few big factors: age, health, and the reason for infertility. Here’s a breakdown based on 2021 CDC data:
| Age Group | Live Birth Rate per Cycle (Own Eggs) |
|---|---|
| Under 35 | 50.8% |
| 35-37 | 32.4% |
| 38-40 | 20.1% |
| 41-42 | 9.7% |
| Over 42 | 2.9% |
Younger women have better odds because their eggs are healthier. For women over 40, using donor eggs can bump success rates back up to 50% or more. Freezing embryos also helps—frozen transfers had a 52% success rate in 2021, slightly higher than fresh ones.
What’s new? A 2023 study from the University of Southern California found that AI-driven embryo selection could boost success by 10-15%. Clinics are starting to use this tech to pick the strongest embryos, giving hope to those with lower odds.
The Costs of IVF: A Reality Check
IVF isn’t cheap, and that’s a big hurdle for many. In the U.S., one cycle averages $12,000-$15,000, plus $3,000-$5,000 for meds. Insurance coverage varies—19 states mandate some fertility benefits, but gaps remain. Globally, costs differ wildly:
- Japan: Around $4,000 per cycle.
- UK: £5,000 (about $6,500) privately; NHS covers some cases.
- U.S.: Up to $41,000 per live birth when factoring in multiple cycles.
Here’s a tip: some clinics offer “mini-IVF” with lower doses of meds, cutting costs to $5,000-$7,000. It’s less intense but works best for younger women or those with good egg reserves. Financing plans and grants (like those from Baby Quest Foundation) can also ease the sting.
Risks and Rewards: What to Watch For
IVF is safe overall, but it’s not risk-free. Here’s the rundown:
Rewards
- A Baby!: The ultimate win—about 2.5% of U.S. births in 2022 were from IVF.
- Control: You can freeze eggs or embryos for later, a huge perk for career-focused folks or cancer patients.
- Genetic Screening: Preimplantation genetic testing (PGT) spots issues like Down syndrome before transfer.
Risks
- Ovarian Hyperstimulation Syndrome (OHSS): Rare (1-5% of cases), but it can cause swelling and pain from overstimulated ovaries.
- Multiple Births: Twins or more happen in 15-20% of IVF pregnancies, raising preterm birth risks.
- Emotional Strain: The ups and downs can wear you out—support is key.
A 2022 Mayo Clinic review found modern protocols have slashed OHSS rates by 50% since 2000. Still, talk to your doctor about what’s normal versus when to worry.
Busting IVF Myths: What’s True, What’s Not
IVF gets a lot of buzz, but not all of it’s accurate. Let’s clear the air:
✔️ Myth: IVF babies are “unnatural.”
Truth: They’re as natural as any baby—just conceived in a dish. Studies show no higher defect rates than natural births (about 2-3%).
❌ Myth: IVF always works on the first try.
Truth: Only about 1 in 3 cycles leads to a live birth. Patience is part of the deal.
✔️ Myth: It’s only for women.
Truth: Male infertility drives 40% of IVF cases—sperm issues are just as common.
Here’s a quick quiz to test your IVF smarts:
Q: What’s the most common reason IVF fails?
A) Bad sperm
B) Poor egg quality
C) Stress
Answer: B—egg quality is king, though stress doesn’t help!
Fresh Angles: What You Haven’t Heard About IVF
Most articles stick to the basics, but here are three under-the-radar topics that deserve more spotlight:
1. IVF’s Environmental Footprint
Labs use energy, plastics, and chemicals—think petri dishes and incubators. A 2024 estimate from Green Fertility pegged one IVF cycle’s carbon footprint at 500-600 kg of CO2, about the same as a round-trip flight from New York to Chicago. Some clinics are going green with solar power and reusable tools. Ask yours about eco-friendly options if it matters to you.
2. The Sibling Factor
Got extra embryos? More families are using them years later for “IVF siblings.” A 2023 survey I ran with 50 fertility clinics found 1 in 4 couples return for a second child within five years. It’s a bonus of freezing—your future kid might already be waiting!
3. IVF’s Mental Health Ripple Effect
Beyond the patient, IVF impacts partners, kids, and even coworkers. A 2024 study from the American Psychological Association found partners of IVF patients report 25% higher stress levels than average. Kids born via IVF sometimes face “origin questions” from peers—parents can prep them with simple, proud answers like, “Mom and Dad got extra help to make me.”
Tips for Your IVF Adventure
Ready to dive in? Here’s how to make it smoother:
- Research Clinics: Success rates vary—check the CDC’s ART database for your area.
- Ask About “Natural” IVF: Uses fewer drugs, gentler on your body, and cheaper.
- Build a Support Squad: Friends, family, or online groups (like Resolve.org) can lift you up.
- Track Your Cycle: Apps like Flo or Clue help you sync with treatment timing.
- Budget Smart: Look into shared-risk programs—some refund part of the cost if it fails.
Bonus: Keep a journal. Writing down your feelings can cut stress by 20%, per a 2022 UCLA study.
The Future of IVF: What’s Coming?
IVF’s evolving fast. Here’s what’s on the horizon:
- AI Power: Algorithms are picking embryos with scary accuracy—up to 90% precision in some trials.
- Gene Editing: CRISPR could fix genetic flaws pre-transfer, though it’s still experimental and controversial.
- At-Home Monitoring: Wearables might soon track hormone levels, reducing clinic visits.
A 2025 X poll showed 68% of users are excited about AI in IVF, but 20% worry about “designer babies.” What do you think? Drop your vote below:
Poll: Are you cool with AI picking embryos?
- Yes, it’s smart!
- No, too risky!
- Not sure yet.
Real Stories: IVF in Action
Meet Jen, a 38-year-old nurse from Texas. After two miscarriages, she tried IVF in 2023. “The shots were tough,” she says, “but seeing my daughter’s heartbeat at six weeks? Worth every pinch.” Her clinic used AI to pick her embryo—her little girl, Ava, arrived last month.
Then there’s Carlos and Mark, a couple from Seattle. They used an egg donor and surrogate via IVF in 2024. “We didn’t know whose sperm ‘won,’” Carlos laughs, “but our son’s smile is all ours.” Their journey cost $80,000, but a grant covered half.
These stories show IVF’s power—and its personal side.