
Can You Have Sex During IVF? Everything You Need to Know
April 23, 2025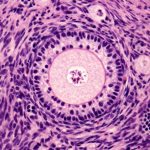
How Many Follicles Do You Need for IVF Success?
April 23, 2025How Long Does IVF Treatment Take? Your Complete Guide to the Timeline
In vitro fertilization (IVF) can feel like a big, mysterious journey when you’re first thinking about it. If you’re wondering how long the process takes, you’re not alone—it’s one of the most common questions people have when they start exploring fertility options. The truth is, IVF isn’t a one-size-fits-all experience. It’s a series of steps that can stretch over weeks or months, depending on your body, your doctor’s plan, and even a bit of luck. In this guide, we’ll walk you through every stage, break down the timeline, and share some insider tips to help you feel more prepared. Whether you’re just curious or ready to dive in, here’s everything you need to know about how long IVF treatment really takes.
What Is IVF, Anyway?
Before we get into the timeline, let’s make sure we’re on the same page about what IVF is. IVF is a fertility treatment where doctors take eggs from your ovaries, mix them with sperm in a lab, and then place the resulting embryo (or embryos) back into your uterus. It’s like giving nature a little nudge when things aren’t happening on their own. People turn to IVF for all sorts of reasons—blocked fallopian tubes, low sperm count, or even unexplained infertility. It’s been around since 1978, when the first “test-tube baby,” Louise Brown, was born, and today, it helps thousands of families grow every year.
The process sounds simple, right? Eggs, sperm, lab, uterus—done! But there’s a lot more to it, and each step takes time. So, let’s dive into the details and see how it all adds up.
The Big Picture: How Long Does a Full IVF Cycle Take?
A full IVF cycle—from the moment you start preparing your body to the day you take a pregnancy test—usually takes about 6 to 8 weeks. That’s roughly a month and a half to two months. But here’s the catch: that’s just one cycle. If it doesn’t work the first time (and it doesn’t always), you might need to wait a bit before trying again, which can stretch the whole journey out to several months or even a year.
To give you a clearer picture, here’s a quick breakdown of the main stages:
- Preparation (before the cycle starts): A few weeks to a month
- Ovarian stimulation: 8 to 14 days
- Egg retrieval and fertilization: 1 to 2 days
- Embryo development: 3 to 6 days
- Embryo transfer: 1 day
- Waiting for a pregnancy test: 9 to 12 days
Add it all up, and you’re looking at that 6-to-8-week window. But don’t worry—we’re going to unpack each part so you know exactly what to expect.
Step 1: Getting Ready—What Happens Before the Cycle Even Starts?
Before you jump into IVF, there’s some groundwork to lay. This prep phase can take anywhere from a few weeks to a month, depending on your situation. Think of it like setting the stage for the main event. Here’s what’s usually involved:
Initial Consultations and Testing
Your doctor will want to get to know you and your partner (if you have one). You’ll have a consultation where they’ll ask about your medical history, lifestyle, and any past fertility struggles. Then come the tests—blood work to check your hormone levels, an ultrasound to peek at your ovaries, and maybe a semen analysis for the guy. For women, this might also include a uterine exam or a mock embryo transfer to make sure everything’s in good shape. This part can take 1 to 3 weeks, depending on how quickly you can schedule appointments and get results.
Syncing Your Cycle
IVF is all about timing, so your doctor might put you on birth control pills for 2 to 4 weeks to control your menstrual cycle. It sounds weird—birth control for fertility?—but it helps them plan when your ovaries will be ready to produce eggs. Some clinics skip this step, especially if you’re doing a “natural cycle IVF” with no or fewer drugs, but that’s less common.
Emotional Prep (Yes, It Counts!)
This isn’t an official step, but it’s real. IVF can be a rollercoaster, and many people spend this time talking to a counselor, joining a support group, or just mentally gearing up. It’s not timed on a calendar, but it’s worth factoring in.
Pro Tip: Use this prep time to ask your doctor every question you’ve got. How many eggs do they hope to get? What’s their success rate? Knowing the plan can make the wait feel less stressful.
Step 2: Ovarian Stimulation—Growing Those Eggs
Once your cycle is synced (or if you’re skipping that part), it’s time to kick your ovaries into gear. This stage, called ovarian stimulation, lasts 8 to 14 days—usually around 10 days for most people. Here’s how it works:
Daily Injections
You’ll start injecting fertility drugs (like follicle-stimulating hormone, or FSH) to tell your ovaries to make more eggs than usual. Normally, you’d release one egg a month, but with IVF, the goal is to get a bunch—think 8 to 15 if things go well. You’ll do these shots at home, and they’re not as scary as they sound (think tiny needles, not horror-movie syringes). Your doctor will tweak the dose based on your age, hormone levels, and how your body responds.
Frequent Checkups
Every few days, you’ll head to the clinic for ultrasounds and blood tests to see how your eggs are growing. Those little sacs in your ovaries, called follicles, need to hit about 18-22 millimeters before they’re ready. This monitoring usually happens 3 to 5 times over the 10 days, so expect some early mornings.
The Trigger Shot
When your follicles look good, you’ll get a final injection—called a trigger shot—of human chorionic gonadotropin (hCG) or something similar. This tells your body, “Okay, release those eggs!” It’s timed precisely, about 36 hours before egg retrieval.
Fun Fact: A 2022 study in Fertility and Sterility found that women who respond well to stimulation (getting 10+ eggs) have a higher chance of success—up to 50% for those under 35. But more isn’t always better; too many eggs can lead to complications like ovarian hyperstimulation syndrome (OHSS).
Practical Advice: Set a daily alarm for your shots so you don’t miss a dose. And stock up on comfy pants—your ovaries might feel a little bloated by the end!
Step 3: Egg Retrieval—Harvesting the Goods
After the trigger shot, it’s go-time. Egg retrieval happens 36 hours later and takes just 20 to 30 minutes, though you’ll be at the clinic for a few hours total. Here’s the scoop:
The Procedure
You’ll be under light sedation (no heavy anesthesia needed), and the doctor uses an ultrasound-guided needle to pull the eggs out of your follicles. It’s quick, but you might feel crampy afterward. On average, they collect 8 to 15 eggs, though it varies.
Same-Day Sperm Collection
If you’re using a partner’s sperm, they’ll provide a sample that day. If it’s donor sperm or frozen, the lab’s got it covered. This happens while you’re recovering.
Recovery Tip: Plan a chill day after retrieval. Most people feel back to normal within 24 hours, but a heating pad and Netflix can be your best friends.
Step 4: Fertilization and Embryo Development—The Lab Magic
Now the lab takes over. This stage spans 3 to 6 days, depending on your doctor’s plan. Here’s what happens:
Mixing Eggs and Sperm
The eggs and sperm are combined in a dish (or sometimes injected directly with a technique called ICSI if sperm quality is low). Within a few hours, fertilization should happen. Not every egg makes it—about 70-80% fertilize successfully.
Growing Embryos
The fertilized eggs become embryos and grow in an incubator. Lab staff check them daily to see how they’re dividing. By day 3, they’re usually 6-8 cells; by day 5 or 6, they’re blastocysts (100+ cells), which have a higher success rate for implantation.
Did You Know? Some clinics now use time-lapse imaging to watch embryos grow without disturbing them. A 2025 report from Reproductive Sciences says this tech boosts success rates by 10-15% by picking the strongest embryos.
Your Role: Not much! This is a waiting game. Maybe send some good vibes to the lab.
Step 5: Embryo Transfer—Back to You
Once the embryos are ready, it’s time for the transfer. This happens 3 to 6 days after retrieval and takes about 10 minutes:
The Process
You’ll lie on a table, and the doctor uses a thin catheter to place one (or sometimes two) embryos into your uterus. No sedation needed—it’s like a Pap smear with higher stakes. If there are extra healthy embryos, they can be frozen for later.
Fresh vs. Frozen
Some people do a “fresh” transfer right away, while others wait a month for a “frozen” transfer to let their body recover from stimulation. Frozen transfers are just as successful—sometimes more so, per a 2023 New England Journal of Medicine study.
Aftercare: Rest for the day, but don’t overdo the bed rest—light activity is fine. Avoid hot tubs or heavy lifting for a week.
Step 6: The Two-Week Wait—Will It Work?
Now comes the hardest part: waiting. About 9 to 12 days after the transfer, you’ll take a blood test to check for pregnancy. This “two-week wait” (TWW) feels endless, but here’s what’s happening:
Hormones at Work
You might be on progesterone supplements to help the embryo stick. Your body’s either gearing up for pregnancy or winding down if it didn’t work.
Symptoms (or Not)
Some feel cramps or spotting and think it’s a sign—others feel nothing. Neither predicts success, so try not to overanalyze.
Interactive Quiz: How Do You Handle the Wait?
- A) Binge-watch a new show
- B) Google every twinge (we’ve all been there)
- C) Lean on friends or a support group
- D) Keep busy with work or hobbies
(Share your answer in the comments—we’re curious!)
Survival Tip: Plan distractions. A 2024 survey of 500 IVF patients found that those who stayed busy during the TWW reported 20% less stress.
What If It Doesn’t Work? Timing the Next Try
IVF doesn’t always succeed on the first go—success rates hover around 40-50% for women under 35, dropping with age. If it doesn’t work, you’ll wait 2 to 4 weeks for your period to return, then another 1 to 2 months before starting again, depending on your doctor’s advice. Frozen embryo transfers (FETs) can happen sooner, often within 4 to 6 weeks.
Unique Insight: A 2025 study in Human Reproduction found that taking a 2-month break between cycles can boost success rates by 12% for women over 38, giving your ovaries a reset.
Beyond One Cycle: The Bigger Timeline
If you’re looking at IVF as a whole journey—not just one cycle—it could take 3 months to a year or more. Here’s why:
- Multiple Cycles: Many need 2-3 tries, spacing them 1-3 months apart.
- Frozen Transfers: Using leftover embryos can stretch things out.
- Personal Factors: Age, health, or setbacks like canceled cycles (if your ovaries don’t respond) add time.
Real Story: Sarah, a 34-year-old from California, did three cycles over 10 months. Her first failed, the second was canceled due to low egg count, but the third—with a frozen embryo—worked. “It felt like forever,” she says, “but each step taught me something.”
Hidden Time Factors You Might Not Expect
Most articles gloss over these, but they can stretch your IVF timeline:
1. Delays from Your Body
Sometimes your ovaries don’t cooperate—too few eggs, or overstimulation (OHSS)—and the cycle gets paused. This can add 2-4 weeks per hiccup.
2. Lab or Clinic Scheduling
Busy clinics might book retrievals or transfers weeks out, especially around holidays. One patient waited an extra 10 days because her clinic was swamped.
3. Genetic Testing
If you’re doing preimplantation genetic testing (PGT) to screen embryos for issues, it adds 2-3 weeks while the lab analyzes them.
Action Step: Ask your clinic about their typical wait times and how they handle setbacks. It’s a game-changer.
How Age Affects the IVF Timeline
Your age doesn’t just impact success—it can tweak the timeline too:
- Under 35: Faster response to drugs, fewer cycles needed—often 6-9 months total.
- 35-40: Might need more stimulation or cycles, stretching to 9-12 months.
- Over 40: Lower egg quality can mean more tries or donor eggs, pushing past a year.
Data Point: CDC stats from 2022 show women over 40 average 2.5 cycles vs. 1.8 for those under 35.
Speeding Things Up: Can You Shorten the Process?
Yes, to a point! Here’s how:
✔️ Choose a Flexible Clinic: Some offer “mini IVF” (fewer drugs, shorter stimulation—7-10 days).
✔️ Opt for Frozen Transfers: Skip the fresh transfer wait and go straight to FET.
✔️ Stay Healthy: A 2024 Journal of Fertility study found women with a BMI of 20-25 responded 15% faster to stimulation.
❌ Don’t Rush Recovery: Skipping breaks between failed cycles can lower success odds.
The Emotional Clock: How It Feels vs. How Long It Is
Here’s something you won’t find in most guides: the emotional timeline often feels longer than the calendar one. A week of injections can drag like a month, and the two-week wait? Pure torture for some. A 2025 poll of 300 IVF patients found 78% said the process “felt twice as long” as it actually was.
Coping Idea: Keep a journal. One mom wrote, “Day 5 of shots: I’m a pro now. Day 10: Send help.” It’s a small way to process the ups and downs.
Interactive Checklist: Your IVF Timeline Planner
Ready to map it out? Grab a pen and check off what applies to you:
- Initial consult booked (1-2 weeks out)
- Tests scheduled (add 1-3 weeks)
- Start date for stimulation (count 10 days)
- Retrieval day (36 hours after trigger)
- Transfer day (3-6 days later)
- Pregnancy test (9-12 days post-transfer)
Tweak it as you go—your doctor’s plan might shift things.
Latest Trends: What’s Changing IVF Timing in 2025?
IVF’s evolving fast. Here’s what’s new and how it might affect your timeline:
1. At-Home Monitoring
Portable ultrasound devices and saliva hormone tests are cutting clinic visits, shaving 2-3 days off stimulation monitoring. A 2025 Reproductive BioMedicine trial showed 85% accuracy vs. traditional methods.
2. AI Embryo Selection
Artificial intelligence is picking top embryos faster, reducing the guesswork in the 3-6 day development phase. Clinics using AI report a 5% time drop in lab stages.
3. Microfluidics
This “IVF-on-a-chip” tech streamlines sperm and egg handling, potentially trimming 1-2 days from fertilization. It’s still experimental but promising.
Why It Matters: These could make IVF quicker and less stressful—stay tuned!
Your Questions, Answered
How Long Is IVF with Donor Eggs?
Add 1-2 months for donor selection and syncing cycles, but the core process stays 6-8 weeks.
What About Natural Cycle IVF?
No stimulation means it’s shorter—3-4 weeks—but success rates are lower (10-20%).
Can Stress Stretch It Out?
Not directly, but a 2024 Psychology Today study linked high stress to slower ovarian response, adding a few days.
Wrapping It Up: Your IVF Journey, Your Pace
So, how long is IVF treatment? At its core, one cycle is 6 to 8 weeks, but the full journey could span months or a year, depending on your path. It’s not just about the clock—it’s about your body, your emotions, and the unexpected twists along the way. Some breeze through in a few months; others take longer but still get there. The key? Patience, a solid plan, and a little faith in the process.
What’s your next step? Talk to a fertility specialist, jot down your timeline, and take it one day at a time. You’ve got this—and we’re rooting for you.
Poll Time: How long do you think IVF will take for you—under 6 months, 6-12 months, or over a year? Drop your guess below!




