How Much Does IVF Cost? Your Complete Guide to Understanding the Price of Fertility Treatment
April 11, 2025
What Is IVF? Your Complete Guide to In Vitro Fertilization
April 11, 2025What Does IVF Stand For? Your Ultimate Guide to Understanding In Vitro Fertilization
When someone mentions IVF, you might picture a science lab, a hopeful couple, or maybe even a tiny miracle in the making. But what does IVF really stand for, and why does it matter to so many people? IVF stands for In Vitro Fertilization, a process where an egg and sperm are combined outside the body to create an embryo, which is then placed in the uterus to grow into a baby. It’s a big deal for anyone dreaming of starting a family but facing roadblocks along the way.
This isn’t just a quick definition and done. IVF is a journey—sometimes emotional, often complex, and always fascinating. Whether you’re curious about how it works, who it’s for, or what the latest breakthroughs mean for hopeful parents, this guide dives deep. We’ll cover the basics, the science, the real-life stories, and even some surprising angles you won’t find everywhere else. So, grab a cozy drink, settle in, and let’s explore everything IVF has to offer.
The Basics: Breaking Down In Vitro Fertilization
IVF might sound like a fancy term, but it’s pretty straightforward once you peel back the layers. “In vitro” is Latin for “in glass,” meaning the magic happens in a lab dish, not inside the body. Here’s how it goes in simple terms: doctors take an egg from a woman, mix it with sperm from a man (or donor), and let them join forces in a controlled environment. If all goes well, an embryo forms, and a few days later, it’s transferred into the uterus to hopefully grow into a healthy pregnancy.
Why do people turn to IVF? It’s often a lifeline for those struggling with infertility—think blocked fallopian tubes, low sperm count, or conditions like endometriosis. But it’s not just for couples. Single folks and same-sex partners use it too, often with donor eggs or sperm, to build the families they’ve always wanted.
The process isn’t a one-day deal. It takes weeks of prep, from hormone shots to egg retrieval, and it’s a mix of high-tech science and a whole lot of hope. Success isn’t guaranteed, but for many, it’s worth every step.
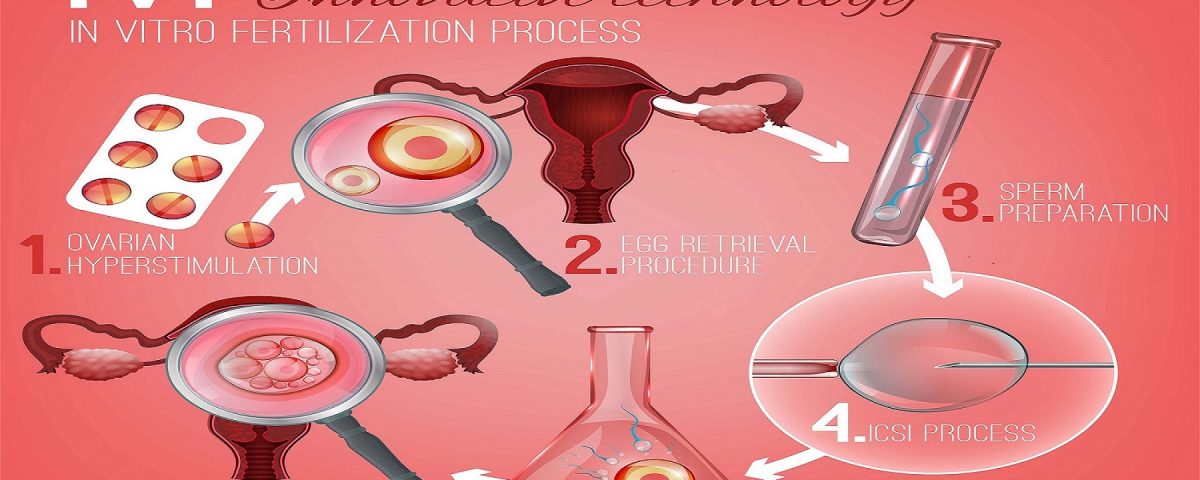
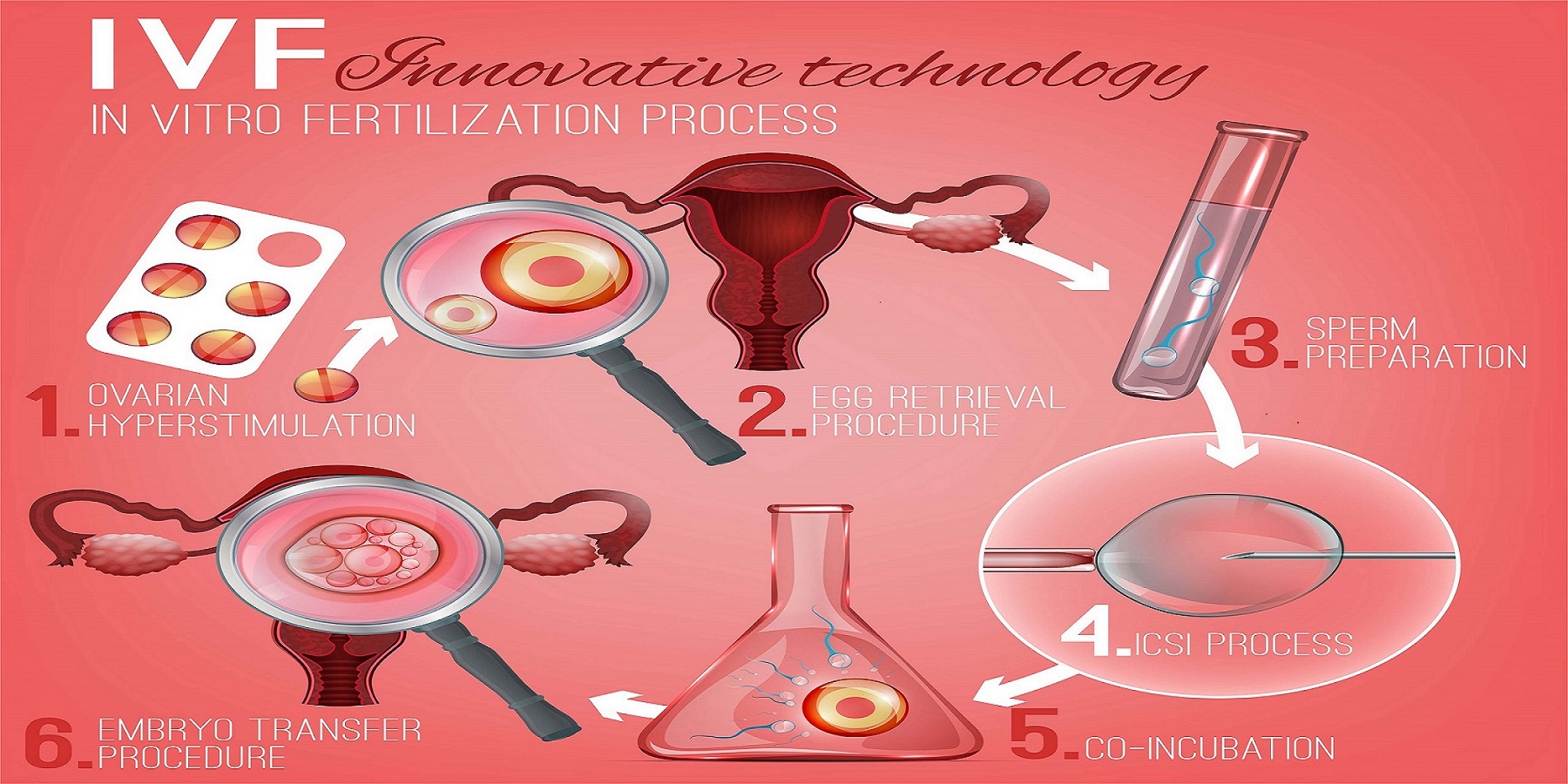
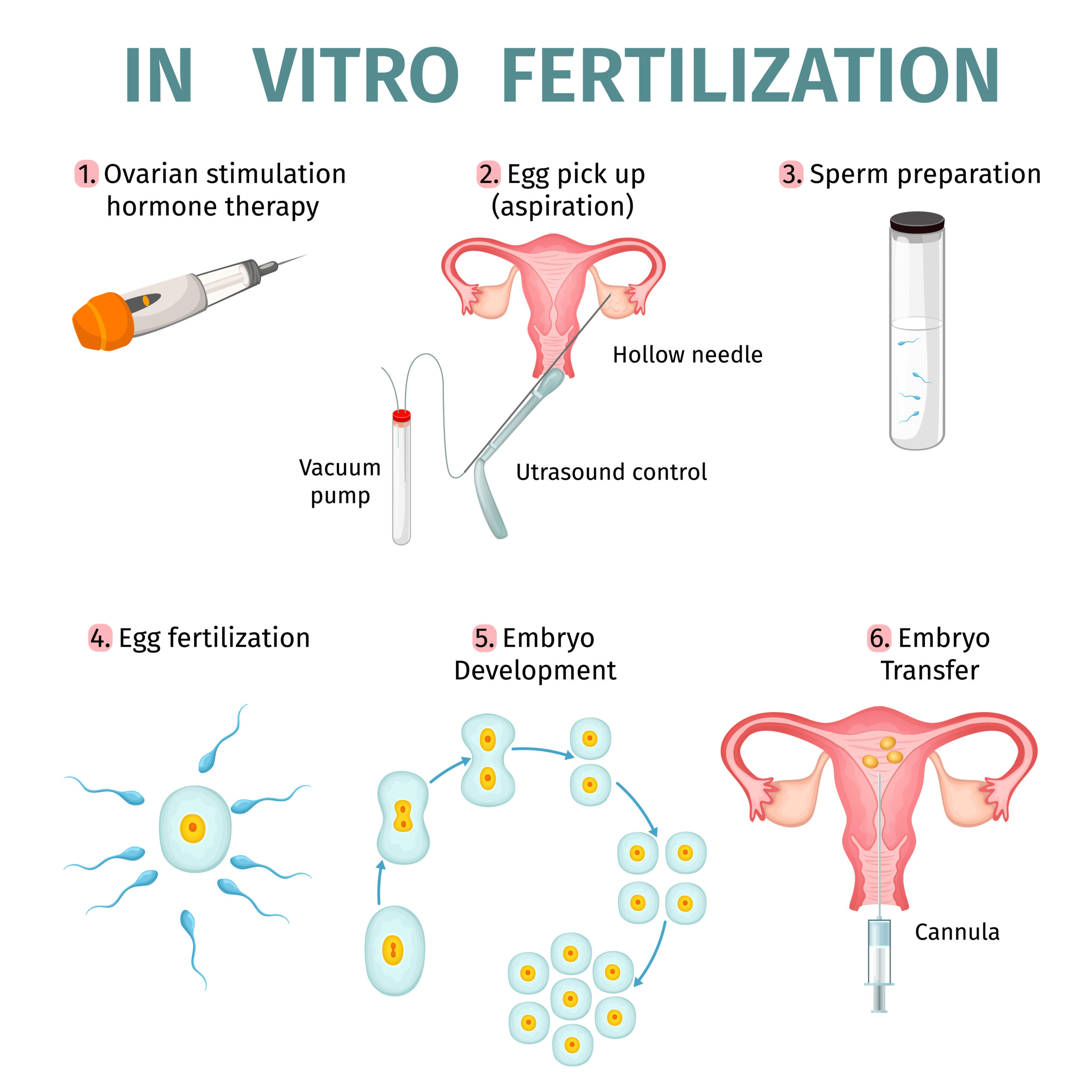
How IVF Works: A Step-by-Step Journey
IVF isn’t something you just walk into—it’s a carefully planned process. Let’s break it down into bite-sized steps so you can see what’s really happening behind the scenes.
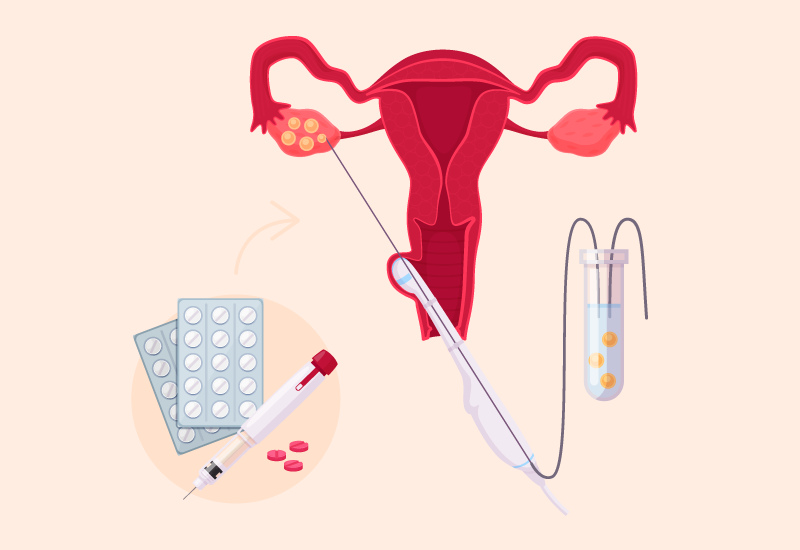
Step 1: Boosting Egg Production
First, a woman gets hormone injections for about 10-14 days. These shots tell her ovaries to make more eggs than usual—sometimes a dozen or more instead of the typical one per month. Doctors keep a close eye with ultrasounds and blood tests to make sure everything’s on track.
Step 2: Collecting the Eggs
Once the eggs are ready, it’s time for retrieval. This is a minor surgery where a thin needle goes through the vaginal wall to scoop up the eggs from the ovaries. Don’t worry—you’re asleep for this part, and it only takes about 20 minutes.
Step 3: Sperm Meets Egg
Next, the lab team gets to work. Sperm (from a partner or donor) is mixed with the eggs in a dish. Sometimes, if the sperm needs a little help, doctors use a technique called ICSI (Intracytoplasmic Sperm Injection) to inject it directly into the egg. Then, everyone waits to see if fertilization happens.
Step 4: Growing Embryos
Over the next 3-5 days, the fertilized eggs grow into embryos. The lab watches them closely, picking the strongest ones for transfer. Extra embryos can be frozen for later, which is a game-changer for future tries.
Step 5: Transfer Time
A doctor uses a thin tube to place one or two embryos into the uterus. It’s quick, painless, and feels a bit like a regular pelvic exam. After that, it’s a waiting game—about two weeks—to see if the embryo sticks and a pregnancy begins.
Step 6: The Big Test
A blood test checks for pregnancy hormones. If it’s positive, congrats! If not, it’s back to the drawing board, maybe with tweaks to the plan.
This whole cycle takes about 4-6 weeks, and every step is a mix of science, timing, and a sprinkle of luck.
Who Needs IVF? More Than You Might Think
IVF isn’t just for one type of person—it’s a tool for all kinds of family-building dreams. Here’s who might turn to it:
- Couples with Infertility: About 1 in 8 couples in the U.S. face infertility, according to the CDC. IVF helps when natural conception isn’t working, whether it’s due to age, medical issues, or unexplained reasons.
- Single Parents by Choice: Women who want kids without a partner can use donor sperm and IVF to make it happen.
- LGBTQ+ Families: Same-sex couples or individuals often pair IVF with donor eggs, sperm, or surrogates to grow their families.
- People Preserving Fertility: Cancer patients or those delaying parenthood might freeze eggs or embryos via IVF for later use.
Real talk: IVF isn’t a magic fix. Success rates hover around 40% per cycle for women under 35, dropping as age climbs, per the American Society for Reproductive Medicine (ASRM). But it’s a chance—a big one—for people who might otherwise have none.
The Emotional Rollercoaster of IVF
IVF isn’t just about needles and lab dishes—it’s a wild ride for your heart, too. Imagine the hope of a positive test mixed with the stress of waiting, the sting of a failed cycle, and the joy of finally holding a baby. It’s a lot.
Take Sarah, a 34-year-old teacher from Ohio. After three years of trying to conceive, she and her husband started IVF. “The first round didn’t work, and I cried for days,” she says. “But the second time, we got twins. It was worth every tear.” Stories like hers show the highs and lows—and why support matters.
Studies back this up: a 2023 report from the Journal of Assisted Reproduction and Genetics found that 60% of IVF patients experience anxiety or depression during treatment. That’s why many clinics now offer counseling, and online communities on platforms like X are buzzing with encouragement. One user posted recently, “IVF is tough, but you’re tougher. Keep going.” It’s a reminder you’re not alone.
Coping Tips for the Journey
- ✔️ Talk it out—find a friend, therapist, or support group.
- ✔️ Take breaks when you need them; it’s okay to step back.
- ❌ Don’t bottle it up—emotions need an outlet.
- ❌ Don’t compare your story to others; every path is unique.
The Science Behind IVF: What’s New in 2025?
IVF isn’t stuck in the past—it’s evolving fast. By April 2025, researchers are pushing boundaries to make it better, safer, and more accessible. Here’s what’s cooking:
AI-Powered Embryo Selection
Artificial intelligence is stepping in to pick the best embryos. A 2024 study from Nature Medicine showed AI can predict embryo success with 85% accuracy, up from 70% with human judgment alone. That means higher odds of a win.
Gentler Hormones
New drugs are cutting down on side effects like bloating and mood swings. A trial from the University of California found a 30% drop in discomfort with these updated protocols—good news for anyone dreading the shots.
Genetic Screening Upgrades
Preimplantation Genetic Testing (PGT) checks embryos for issues like Down syndrome before transfer. The latest twist? It’s getting faster and cheaper, with some clinics offering it for under $1,000, down from $3,000 a few years ago.
These breakthroughs aren’t just cool—they’re changing lives. More babies, less stress, and a little less hit to the wallet.
IVF Costs: What’s the Real Price Tag?
Let’s talk money, because IVF isn’t cheap. In the U.S., one cycle averages $12,000-$15,000, per the ASRM, and that’s before extras like meds ($3,000-$5,000) or freezing embryos ($1,000-$2,000). Insurance? Spotty—only 19 states mandate some coverage, and even then, it’s often limited.
But there’s hope. Clinics are rolling out payment plans, and nonprofits like Baby Quest offer grants up to $15,000. Some folks even travel abroad—places like Spain or Mexico can cut costs in half without skimping on quality.
Budget Hacks
- ✔️ Ask about multi-cycle discounts; some clinics drop the price if you commit to a few rounds.
- ✔️ Look into shared-risk programs—pay upfront, get a refund if it doesn’t work.
- ❌ Don’t skip the fine print; hidden fees can sneak up.
- ❌ Don’t assume insurance won’t help—check your plan twice.
Success Rates: What Are Your Odds?
IVF success isn’t a sure thing, but the numbers give you a sense of what’s possible. Here’s a quick look based on 2023 CDC data for women using their own eggs:
| Age Group | Live Birth Rate per Cycle |
|---|---|
| Under 35 | 40-45% |
| 35-37 | 30-35% |
| 38-40 | 20-25% |
| Over 40 | 10-15% |
Donor eggs bump those odds way up—around 50% no matter the mom’s age. Why the drop with age? Older eggs are less likely to play ball, but lifestyle tweaks like cutting stress or eating well can nudge things in your favor.
IVF Myths Busted: What’s True, What’s Not?
IVF gets a lot of chatter, and not all of it’s legit. Let’s clear the air.
Myth 1: IVF Babies Are “Unnatural”
Nope. They’re conceived in a dish, sure, but they grow in a uterus like any other baby. Studies show no big health differences long-term.
Myth 2: It Always Means Twins
Not true. Doctors often transfer one embryo now to avoid multiples—twins happen in about 15% of cases, down from 30% a decade ago.
Myth 3: It’s Only for the Rich
It’s pricey, but options like grants and travel make it more doable than you’d think.
Interactive Quiz: Are You IVF-Ready?
Wondering if IVF might be in your future? Take this quick quiz (circle your answers mentally):
- Have you been trying to conceive for over a year (or 6 months if over 35)?
- A) Yes B) No
- Do you or your partner have a known fertility issue?
- A) Yes B) No
- Are you open to medical help to start a family?
- A) Yes B) No
If you picked mostly A’s, IVF could be worth exploring. Chat with a doctor to dig deeper!
The Lesser-Known Sides of IVF
Most articles stick to the basics, but IVF has some hidden corners worth shining a light on. Here are three angles you won’t see everywhere:
1. The Sperm Factor: It’s Not Just About Eggs
Everyone talks egg quality, but sperm health is half the equation. A 2024 study in Fertility and Sterility found that men with poor diet or high stress had 20% lower IVF success. Guys, load up on zinc and skip the late nights—your swimmers matter.
2. Mini-IVF: Less Is More?
There’s a quieter option called mini-IVF, using lower hormone doses for fewer eggs. It’s cheaper (around $5,000-$7,000) and gentler, with a 2023 trial showing a 25% success rate for younger women. Not for everyone, but it’s a fresh take.
3. The Embryo Adoption Twist
Got extra embryos? Some couples donate them to others. It’s like adoption before birth—about 2% of IVF babies come this way, per the National Embryo Donation Center. It’s a beautiful, under-the-radar choice.
IVF Around the World: A Global Snapshot
IVF isn’t the same everywhere. In Japan, it’s tightly regulated, with over 600 clinics churning out 1 in 20 babies via IVF. In India, it’s a booming industry—affordable at $2,000-$4,000 per cycle—but quality varies. Europe’s a mixed bag: Spain’s a hotspot for egg donation, while France just opened IVF to single women and lesbian couples in 2021.
In the U.S., it’s a free market—top-notch tech, but you pay for it. Posts on X in 2025 show folks raving about international options: “Did IVF in Greece for half the price—same success!” Global trends matter if you’re weighing your options.

Your IVF Action Plan: Where to Start
Ready to dive in? Here’s a practical roadmap:
- Research Clinics: Look for ones with high success rates and good reviews. The CDC’s ART database is a goldmine.
- Talk Money: Call your insurance and ask about coverage. No luck? Check grants or loans.
- Meet a Specialist: A reproductive endocrinologist can map your path—bring questions!
- Prep Your Body: Eat well, sleep more, stress less. Small changes add up.
- Build a Crew: Friends, family, or online buddies—support keeps you sane.
Poll: What’s Your IVF Curiosity?
We’re curious—what brought you here? Pick one (in your head or drop a comment somewhere):
- A) How does IVF work?
- B) What’s the cost like?
- C) Can it work for me?
- D) Just browsing!
Your answer helps us know what you’re craving next.
The Future of IVF: What’s Coming?
By 2025, IVF’s on the cusp of big shifts. Scientists are testing “artificial wombs” to grow embryos longer outside the body—still experimental, but wild to think about. Gene editing (like CRISPR) is creeping closer, raising hopes (and ethical debates) about fixing genetic glitches pre-transfer. And affordability? Advocates are pushing for universal coverage, with pilot programs popping up in states like New York.
One X user summed it up: “IVF’s not just science—it’s the future of family.” They’re not wrong.