How Much Does IVF Cost in Texas?
April 17, 2025
What Is the IVF Process? Your Complete Guide to In Vitro Fertilization
April 18, 2025What Is IVF? Your Complete Guide to In Vitro Fertilization
In vitro fertilization, or IVF, is a term you might have heard tossed around in conversations about starting a family, especially when things don’t go as planned. Maybe you’ve seen it in a movie, read about a celebrity using it, or even know someone who’s gone through it. But what exactly is IVF? At its core, it’s a way to help people have a baby when nature needs a little nudge. It’s not magic, but it can feel like a miracle to those who’ve struggled with infertility. In this guide, we’re diving deep into what IVF is, how it works, who it’s for, and what you can expect—plus some fresh insights you won’t find everywhere else.
IVF has been around since the late 1970s, when the first “test-tube baby,” Louise Brown, was born in England. Since then, it’s helped millions of people worldwide become parents. Today, it’s more advanced, more accessible, and packed with options to fit different needs. Whether you’re just curious or seriously considering it, this article will walk you through everything in a way that’s easy to grasp, with a few surprises along the way.
The Basics: What Does IVF Mean?
IVF stands for “in vitro fertilization.” Let’s break that down. “In vitro” is Latin for “in glass,” meaning the process happens outside the body, usually in a lab dish. “Fertilization” is when a sperm and egg join to start a pregnancy. So, IVF is about taking those two ingredients—sperm and egg—mixing them in a lab, and then placing the resulting embryo into the uterus to grow into a baby. Simple, right? Well, not quite—it’s a multi-step journey, and each part has its own challenges and triumphs.
Think of IVF like baking a cake. You gather the ingredients (eggs and sperm), mix them in a special environment (the lab), and then put the batter (the embryo) into the oven (the uterus) to finish. Except this cake takes nine months to “bake” and comes with a lot more emotions!
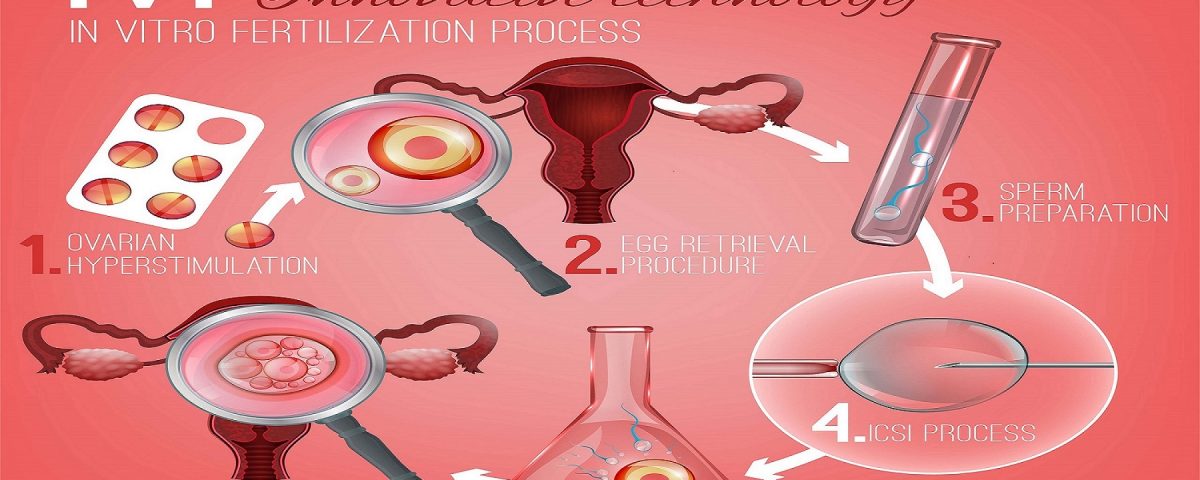
How Does IVF Work? A Step-by-Step Look
IVF isn’t a one-and-done deal—it’s a process with several stages. Here’s how it typically goes, explained so you can picture it without getting lost in medical jargon.
Step 1: Boosting Egg Production
First, a woman takes fertility drugs to help her ovaries produce more eggs than usual. Normally, your body releases one egg a month, but IVF needs a bigger batch to increase the chances of success. These meds are usually shots or pills, and they work by telling your ovaries, “Hey, let’s get busy!” Doctors keep a close eye on this with ultrasounds and blood tests to make sure everything’s on track.
- How long? About 10-14 days.
- What’s it like? You might feel bloated or moody—kind of like PMS on steroids.
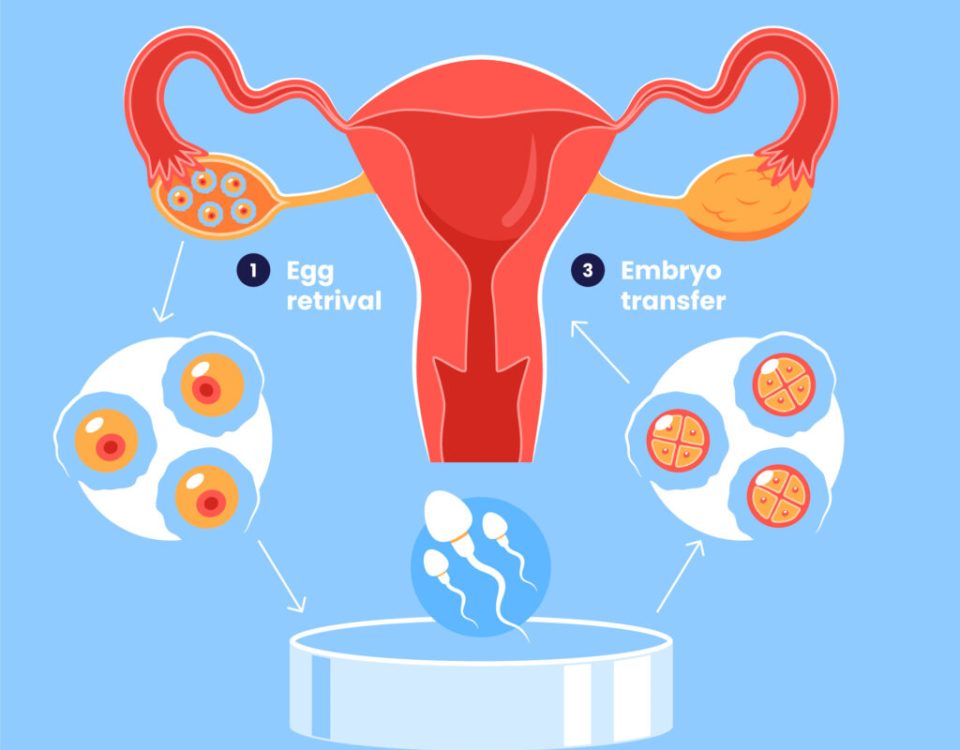
Step 2: Collecting the Eggs
Once the eggs are ready, it’s time to grab them. This happens in a quick procedure called egg retrieval. A doctor uses a thin needle, guided by ultrasound, to pull the eggs out of the ovaries through the vagina. You’re usually sedated, so it’s not as scary as it sounds—more like a nap with a purpose.
- Timeframe: Takes about 20-30 minutes.
- Recovery: Rest for a day, and you’re usually good to go.
Step 3: Fertilizing the Eggs
Now the lab takes over. The eggs meet the sperm in a dish, and fertilization happens. Sometimes, if the sperm needs help, doctors use a technique called ICSI (intracytoplasmic sperm injection), where they inject a single sperm right into an egg. After a day or two, the fertilized eggs become embryos—tiny bundles of cells with big potential.
- Fun fact: Embryos start as just a few cells, smaller than a grain of sand!
Step 4: Growing the Embryos
The embryos hang out in the lab for 3-5 days, growing stronger. Scientists watch them closely, picking the healthiest ones for the next step. Any extras can be frozen for later, like saving leftovers for another meal.
Step 5: Transferring the Embryo
Finally, one or two embryos are placed into the uterus using a thin tube called a catheter. It’s a simple process—no anesthesia needed—and feels a bit like a Pap smear. If the embryo sticks to the uterine lining (called implantation), pregnancy begins!
- When do you know? A pregnancy test about 10-14 days later tells the tale.
Who Can IVF Help?
IVF isn’t just for one type of person—it’s a tool for all kinds of situations. Here’s who might turn to it:
- Couples with infertility: If you’ve been trying for a year (or six months if you’re over 35) without luck, IVF might be an option. Blocked fallopian tubes, low sperm count, or unexplained issues are common reasons.
- Same-sex couples or single folks: Using donor eggs, sperm, or a surrogate, IVF opens doors to parenthood.
- People with genetic concerns: IVF can screen embryos for certain conditions, helping avoid passing them on.
- Women with age-related fertility drops: As eggs age, IVF can use donor eggs or frozen ones from earlier years.
Real story: Take Sarah, a 38-year-old teacher I heard about. After years of irregular periods and no pregnancies, she learned her fallopian tubes were scarred. IVF gave her a shot, and after two rounds, she welcomed twins. It’s not always that smooth, but it shows what’s possible.
What Are the Success Rates?
Success isn’t guaranteed with IVF—it depends on a lot. Age is the biggest factor. According to the CDC’s 2022 data, here’s a snapshot:
| Age Group | Success Rate (Live Birth per Cycle) |
|---|---|
| Under 35 | About 55% |
| 35-37 | Around 40% |
| 38-40 | Roughly 26% |
| Over 40 | About 8% |
Other things like lifestyle (smoking cuts chances), clinic quality, and specific health issues play a role too. Multiple cycles can boost your odds, but it’s a marathon, not a sprint.
Quick Quiz: What’s Your IVF IQ?
Let’s make this fun! Answer these quick questions:
- What’s the first step in IVF?
A) Egg retrieval B) Fertility drugs C) Embryo transfer - How long does an embryo grow in the lab?
A) 1 day B) 3-5 days C) 2 weeks - What’s the success rate for women under 35?
A) 10% B) 55% C) 90%
(Answers: 1-B, 2-B, 3-B. How’d you do?)
The Emotional Side of IVF
IVF isn’t just physical—it’s an emotional rollercoaster. The hope of a positive test can lift you up, but a negative result can hit hard. Studies show about 40% of people going through IVF deal with anxiety or depression at some point. It’s normal to feel overwhelmed.
- Tip: Talk it out. Friends, a counselor, or online groups (like on X) can be lifelines. One woman I read about said joining a fertility forum made her feel less alone—like having a virtual coffee date with people who get it.
Costs and Coverage: What to Expect
IVF isn’t cheap. In the U.S., one cycle averages $15,000-$20,000, including meds and tests. Insurance varies—some states mandate coverage, but many don’t. Globally, costs differ: in the UK, it’s about £5,000 ($6,500), while in India, it can dip below $3,000.
- Money-saving hack: Look into clinics with “shared risk” programs. You pay upfront for multiple cycles, and if it doesn’t work, you get a refund. It’s like a safety net for your wallet.
Risks and Realities
IVF is safe overall, but it’s not risk-free. Here’s what to watch for:
- Ovarian Hyperstimulation Syndrome (OHSS): Rare (less than 5% of cases), but it can cause swelling and pain from overstimulated ovaries. Mild cases need rest; severe ones might mean a hospital stay.
- Multiple births: Twins or more happen in about 20% of IVF pregnancies, raising risks like preterm birth.
- Emotional toll: Stress is real, and it’s okay to seek help.
A 2023 study from the Journal of Fertility found that tweaking medication doses could cut OHSS rates by 15%—a small but hopeful update not widely covered yet.
Fresh Angles: What You Haven’t Heard About IVF
Most articles stick to the basics, but let’s explore some under-the-radar topics that add depth.
The Role of Lifestyle Tweaks
Sure, you’ve heard “eat healthy,” but did you know specific changes can matter? A 2024 study in Reproductive Health found women who cut caffeine to under 100 mg daily (about one coffee) during IVF had a 10% higher implantation rate. Small swaps—like herbal tea for lattes—might tip the scales.
- Try this: Swap processed snacks for nuts or fruit. Omega-3s in walnuts could boost egg quality, per early research.
Mini IVF: A Gentler Option
Not every IVF cycle needs a full-on approach. Mini IVF uses lower drug doses, aiming for fewer but higher-quality eggs. It’s cheaper (around $5,000-$7,000) and easier on the body, ideal for women sensitive to meds or over 40. Success rates are lower—about 20% per cycle—but it’s a game-changer for some.
- Case in point: Lisa, 42, opted for mini IVF after standard rounds failed. She got pregnant on her second try with less stress and cost.
The Sperm Factor: Beyond the Count
We talk eggs a lot, but sperm health is half the equation. A 2025 X discussion highlighted how heat exposure—like hot tubs or tight pants—can tank sperm quality during IVF prep. One guy switched to loose boxers and saw his sperm motility jump 25% in three months. Little moves, big impact.
- Action step: Guys, keep it cool down there—literally. Skip the sauna for a few months.
Your IVF Prep Checklist
Ready to dive in? Here’s a practical guide to get started:
✔️ Find a clinic: Look for board-certified docs and high success rates. Check reviews on X or forums for real feedback.
✔️ Ask about options: Donor eggs, mini IVF, or freezing embryos—know what fits you.
✔️ Get your body ready: Eat balanced meals, sleep well, and cut stress where you can.
✔️ Talk money: Call your insurance and the clinic for a clear cost breakdown.
❌ Don’t rush: Take time to research and feel confident in your choice.
The Future of IVF: What’s Coming?
IVF keeps evolving. Here’s what’s on the horizon, based on 2025 trends:
- AI in embryo selection: Algorithms are getting better at picking winners, potentially boosting success by 10-15%, per a Nature study.
- At-home monitoring: New devices let you track hormones from home, cutting clinic visits.
- Affordable access: Nonprofits are pushing for lower costs, especially in underserved areas.
Imagine a world where IVF is as routine as a dental checkup—tech is heading that way.
Poll: What’s Your Take?
Let’s hear from you! Pick one:
- IVF sounds exciting—I’d try it if I needed to.
- It’s too complicated or pricey for me.
- I’m just here to learn, no plans yet.
(Comment your choice below—I’m curious!)
Wrapping It Up: Is IVF Right for You?
IVF is a powerful tool, but it’s not a one-size-fits-all fix. It’s about hope, science, and a bit of grit. Whether it’s overcoming blocked tubes, building a family your way, or beating the odds of age, it’s a path worth exploring if it fits your story. The key? Arm yourself with info, lean on support, and trust your gut.
Got questions? Clinics, friends who’ve been there, or even a quick X search can spark answers. IVF’s been changing lives for over 40 years—and with new twists like mini IVF or lifestyle hacks, it’s only getting better. What’s your next step? Maybe it’s just reading this again—or maybe it’s making a call. Either way, you’re not alone on this journey.