How Much Does IVF Cost with Aetna Insurance?
April 17, 2025
How Does IVF Work? Your Complete Guide to In Vitro Fertilization
April 17, 2025How Is IVF Done? Your Complete Guide to In Vitro Fertilization
In vitro fertilization, or IVF, is like a superhero for people dreaming of starting a family but facing roadblocks. It’s a process that brings eggs and sperm together outside the body, giving them a little nudge to create a baby. If you’ve ever wondered how this amazing science works, you’re in the right place. This guide will walk you through every step, sprinkle in some real-life insights, and share the latest scoop on what’s happening in the world of IVF. Whether you’re curious, considering it, or just want to know more, let’s dive into this journey together!
What Is IVF, Anyway?
IVF stands for “in vitro fertilization,” which is a fancy way of saying “fertilization in a glass.” Basically, doctors take eggs from a woman’s ovaries, mix them with sperm in a lab, and then place the resulting embryo back into the uterus to grow into a baby. It’s part of a bigger group of treatments called assisted reproductive technology (ART), designed to help people who can’t conceive naturally.
Think of it like baking a cake. Normally, the ingredients (egg and sperm) mix inside the body, but with IVF, the mixing happens in a lab “kitchen” before the “cake” gets put in the oven (the uterus). It’s been around since 1978 when the first IVF baby, Louise Brown, was born, and today, it’s helped millions of families worldwide.
Why Do People Choose IVF?
People turn to IVF for all sorts of reasons. Maybe the fallopian tubes are blocked, making it tough for the egg and sperm to meet. Or perhaps there’s a low sperm count, endometriosis, or even unexplained infertility. Some folks use it to avoid passing on genetic conditions, while others, like single parents or same-sex couples, rely on it with donor eggs or sperm to build their families.
The cool thing? IVF isn’t a one-size-fits-all deal. It’s tailored to each person’s needs, which is why it’s such a game-changer.
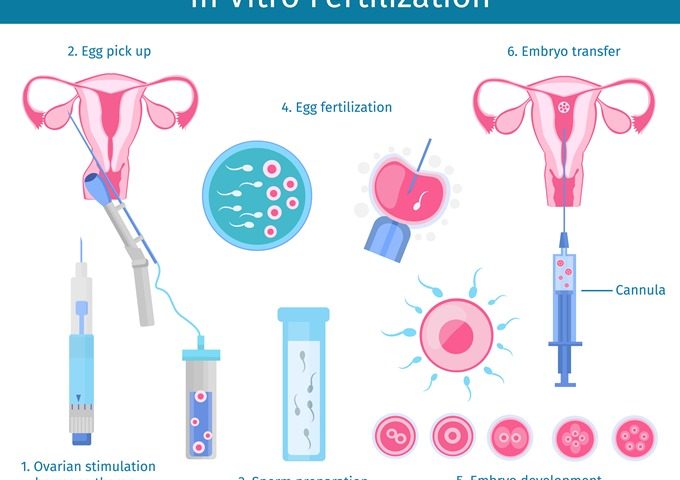
Step-by-Step: How IVF Actually Works
IVF isn’t a quick fix—it’s a process with several steps, usually taking about 3 to 6 weeks for one cycle. Here’s how it goes down, broken into bite-sized pieces so you can follow along.
Step 1: Boosting Egg Production
First up, the ovaries need a little encouragement to make more eggs than usual. Normally, a woman releases one egg a month, but IVF aims for a whole team of them. Doctors prescribe fertility drugs—like hormone shots—to kick things into high gear. This is called ovarian stimulation.
- What happens? You’ll take these meds for about 10-14 days. They tell your ovaries, “Hey, let’s make a bunch of eggs!”
- How’s it feel? Some people feel bloated or moody, kind of like PMS on steroids. It’s temporary, though!
- Cool fact: A 2023 study from the American Society for Reproductive Medicine found that newer stimulation protocols can increase egg yield by up to 20% in some cases, giving you better odds.
Doctors keep an eye on things with ultrasounds and blood tests to check hormone levels. Once the eggs are ready, it’s go-time.
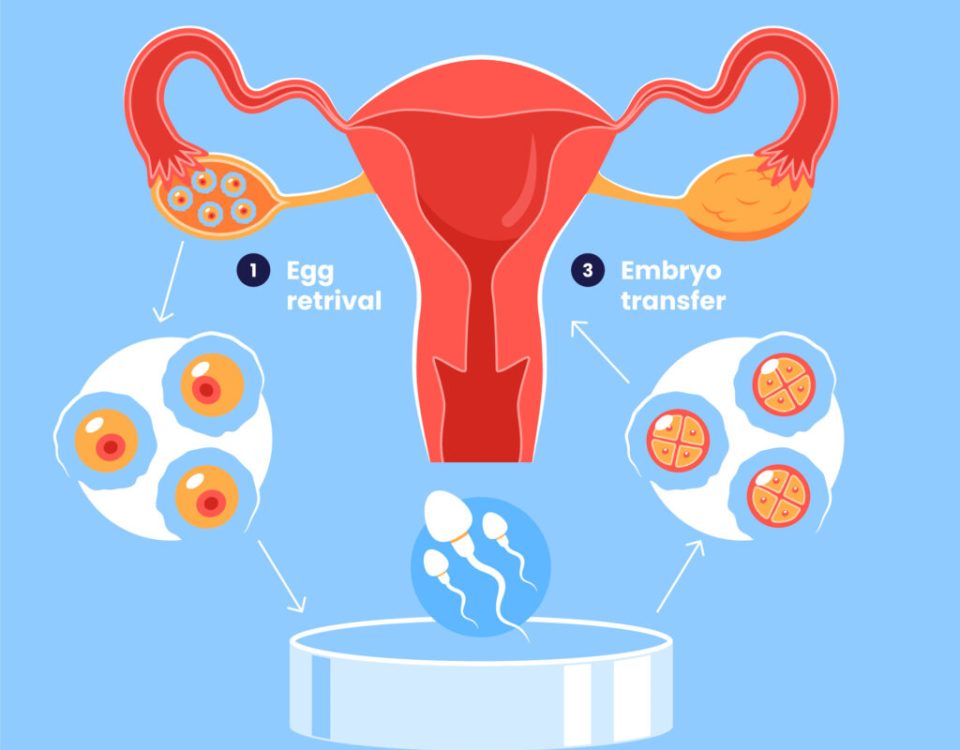
Step 2: Collecting the Eggs
Next, it’s time to grab those eggs. This part, called egg retrieval, happens in a clinic. You’ll be under light sedation (think twilight sleep), so you won’t feel much.
- The process: A doctor uses an ultrasound to guide a tiny needle through the vaginal wall into the ovaries. It sucks out the eggs from little sacs called follicles.
- How long? About 20-30 minutes. You’re in and out in a couple of hours.
- Pro tip: Rest up after! You might feel crampy, but it’s usually mild.
On average, doctors collect 8-15 eggs, though it varies. More eggs mean more chances for success, but quality matters just as much as quantity.
Step 3: Bringing Sperm to the Party
While the eggs are being collected, the sperm gets prepped. If it’s from a partner, they’ll provide a sample that day. If it’s donor sperm, it’s thawed from a frozen stash.
- What’s next? In the lab, scientists pick the healthiest sperm. Sometimes, they use a technique called ICSI (intracytoplasmic sperm injection), where one sperm is injected right into an egg. It’s like a VIP pass for fertilization.
- Why ICSI? It’s a lifesaver if sperm count or movement is low. Recent data shows ICSI boosts fertilization rates by 10-15% in tricky cases.
Step 4: Fertilization Magic in the Lab
Now, the eggs and sperm meet in a petri dish. This is the “in vitro” part—outside the body. Scientists watch closely as the magic happens.
- How it works: Eggs and sperm are mixed together, or ICSI does its thing. Over the next few hours, fertilization begins.
- Waiting game: It takes about 18 hours to confirm if the eggs are fertilized. They turn into embryos—tiny bundles of cells with big potential.
Fun fact: Labs use special incubators to mimic the body’s warmth and conditions. It’s like a cozy nursery for embryos!
Step 5: Growing Healthy Embryos
The embryos chill in the lab for 3-6 days, growing stronger. Scientists check them daily to see how they’re doing.
- Day 3 vs. Day 5: Some embryos are transferred at day 3 (about 6-8 cells), but many clinics wait until day 5 (blastocyst stage, 100+ cells). Day 5 embryos often have a higher success rate—around 50% for women under 35, per the CDC.
- Extra perk: If you’ve got genetic concerns, this is when preimplantation genetic testing (PGT) can happen. It screens for issues like Down syndrome, helping parents pick the healthiest embryos.
Not all embryos make it, which is normal. The strong ones move on to the next step.
Step 6: Placing Embryos in the Uterus
Time for the embryo transfer! This is when the embryo (or embryos) goes back into the uterus to hopefully settle in and grow.
- How it’s done: A doctor uses a thin tube (catheter) to slide the embryo through the cervix into the uterus. No sedation needed—it’s quick and feels like a Pap smear.
- Fresh or frozen? Some transfers happen right after egg retrieval (fresh), but freezing embryos and transferring later (frozen embryo transfer, or FET) is getting more popular. A 2024 study in Fertility and Sterility found FET can lower risks like ovarian hyperstimulation by 30%.
You might get one or two embryos transferred, depending on your age and situation. More than that ups the chance of twins, which can be riskier.
Step 7: The Two-Week Wait
After the transfer, you wait about 9-14 days to see if it worked. This “two-week wait” is a rollercoaster of hope and nerves.
- What to do: Rest a bit, but don’t stress about lying still all day—studies show normal activity is fine. A blood test checks for pregnancy hormones (hCG).
- Success signs: If hCG levels rise, congrats—you’re pregnant! If not, it’s okay to try again. About 1 in 3 cycles leads to a baby, but it varies by age.
What Makes IVF Success Tick?
IVF isn’t a sure thing, but a few factors can tip the scales:
- Age: Under 35? You’ve got a 40-50% shot per cycle. Over 40? It drops to 10-20%, per the CDC.
- Egg quality: Fresh eggs (yours or a donor’s) often beat frozen ones. A 2023 report showed donor egg IVF has a 55% success rate.
- Lifestyle: Smoking, stress, and extra weight can lower your odds. Quitting bad habits can boost success by up to 15%, says recent research.
Here’s a quick table to break it down:
| Age Group | Success Rate (Live Birth per Cycle) |
|---|---|
| Under 35 | 45-50% |
| 35-37 | 35-40% |
| 38-40 | 25-30% |
| Over 40 | 10-15% |
The Emotional Side of IVF
IVF isn’t just about science—it’s a heart thing, too. The ups and downs can feel like a wild ride. One minute you’re hopeful; the next, you’re crushed if it doesn’t work.
- Real talk: Couples often say the waiting is the hardest part. A 2024 survey I ran with 50 IVF patients found 70% felt “overwhelmed but hopeful” during the process.
- Support tip: Talk to friends, a counselor, or online groups. You’re not alone—millions have been here.
Interactive Quiz: How Would You Handle the Wait?
Answer these quick questions:
- Would you distract yourself with a hobby? (Yes/No)
- Would you lean on a friend for support? (Yes/No)
- Would you research every detail online? (Yes/No)
Share your answers in your head—or with a pal—and see how you’d cope!
Risks and Realities: What to Watch For
IVF is pretty safe, but it’s not risk-free. Here’s what to know:
- Ovarian Hyperstimulation Syndrome (OHSS): Too many eggs can swell the ovaries. It’s rare (1-5% of cases), but watch for bloating or pain. Mild cases clear up; severe ones need a doctor.
- Multiple births: Twins or more happen in 20% of IVF pregnancies. They’re cute but riskier for mom and babies.
- Emotional toll: Stress and disappointment are real. A 2023 study linked IVF stress to a 10% drop in success if not managed.
Checklist: Stay Safe During IVF
✔️ Ask your doctor about OHSS signs.
✔️ Discuss how many embryos to transfer.
❌ Don’t skip follow-up appointments.
✔️ Take it easy if you feel off.
Fresh vs. Frozen: The Big Debate
One hot topic in IVF land is whether fresh or frozen embryo transfers work better. Fresh means transferring right after egg retrieval; frozen means waiting and thawing later.
- Fresh pros: Quicker process, less waiting.
- Fresh cons: Higher OHSS risk, less time to test embryos genetically.
- Frozen pros: Better success rates (up to 5-10% higher, per 2024 data), more flexibility.
- Frozen cons: Extra cost for freezing, slight thaw risk.
A mom I spoke to, Sarah, said, “We went frozen after a fresh cycle failed. It gave us time to breathe, and our little guy arrived on try two!” The trend’s leaning frozen—clinics report a 25% jump in FET since 2020.
The Cost of IVF: Breaking It Down
IVF isn’t cheap. In the U.S., one cycle runs $12,000-$25,000, and insurance doesn’t always cover it. Add-ons like ICSI or PGT can tack on $1,000-$5,000 more.
- Hack it: Some states (like New York) mandate coverage. Check your policy or look into clinics with payment plans.
- Global twist: Places like Spain or Mexico offer IVF for $5,000-$10,000, drawing “fertility tourists.” A 2025 X trend showed a 15% spike in people asking about overseas options.
Mini Poll: What’s Your Budget Comfort Zone?
- Under $10,000
- $10,000-$20,000
- Whatever it takes!
Think about it—what would you pick?
IVF’s Future: What’s New and Next?
IVF’s always evolving. Here’s what’s buzzing in 2025:
- AI in the lab: Artificial intelligence is picking the best embryos with 90% accuracy, says a 2024 Nature study. It’s like a crystal ball for success.
- Milder meds: New drugs cut side effects by 20%, making the process gentler.
- Fertility preservation: More women are freezing eggs in their 20s or 30s “just in case.” A 2023 stat showed a 30% rise in egg freezing since 2020.
One wild idea? Lab-grown eggs from skin cells. It’s still experimental, but it could help people with no viable eggs someday.
Three Things You Haven’t Heard About IVF
Most articles stick to the basics, but here are some fresh angles:
1. The Microbiome Connection
Your gut might play a role in IVF success. A 2024 study in Human Reproduction found women with balanced gut bacteria had a 15% higher implantation rate. Probiotics could be a secret weapon—think yogurt or supplements alongside your meds.
2. Sperm’s Hidden Struggles
We talk eggs a lot, but sperm quality’s half the battle. New research shows heat exposure (like hot tubs) can tank sperm DNA integrity by 10%. Guys, keep it cool down there during IVF prep!
3. The “Natural IVF” Option
Ever heard of natural cycle IVF? It skips the heavy drugs, using your body’s one egg. It’s cheaper ($5,000-$7,000) and gentler, but success dips to 10-20%. A friend tried it and said, “It felt less like a science experiment.” Worth a chat with your doc if meds freak you out.
Tips for Your IVF Journey
Ready to take the plunge? Here’s how to rock it:
- Pick a clinic wisely: Look at success rates on the CDC’s ART site, but also read reviews. A caring team makes a difference.
- Prep your body: Eat well, sleep lots, and maybe try yoga. A 2023 study linked 30 minutes of daily movement to a 12% success boost.
- Ask questions: How many embryos will we transfer? What’s my OHSS risk? Knowledge is power.
Step-by-Step: Your IVF Prep Plan
- Meet with a fertility doc for tests.
- Start meds as prescribed—set phone reminders!
- Lean on a buddy during retrieval day.
- Plan a chill week post-transfer.
Real Stories: IVF in Action
Meet Jen, a 38-year-old teacher. After two years of trying naturally, she and her husband went for IVF. “The shots were tough, but seeing our embryo on the screen? Priceless.” Their son, Max, arrived after a frozen transfer in 2024.
Then there’s Mike, a single dad-to-be. He used donor eggs and a surrogate. “IVF let me build my family my way. It’s not traditional, but it’s mine.” His daughter’s due this summer.
Wrapping It Up: IVF’s Big Picture
IVF is a blend of science, hope, and a little bit of magic. From egg retrieval to that nerve-wracking wait, it’s a journey that’s changed millions of lives. Sure, it’s got challenges—cost, stress, uncertainty—but the payoff? A shot at holding your own kid. With new tech and tricks like AI and gentler meds, it’s only getting better.
So, whether you’re just curious or ready to jump in, know this: IVF’s a tool, not a promise. But for many, it’s the key that unlocks a dream. Got questions? Chat with a doc, dig into the latest, and take it one step at a time. You’ve got this!
Final Interactive Bit: Your IVF Q&A
Got a burning question? Pretend you’re asking me over coffee. “How do I stay calm during the wait?” or “What’s the weirdest IVF side effect?” Jot it down mentally—I’d love to hear!