Does Insurance Cover IVF? Your Guide to Understanding Coverage, Costs, and Options
April 11, 2025
How Much Does IVF Cost? Your Complete Guide to Understanding the Price of Fertility Treatment
April 11, 2025What Is IVF Treatment?
In vitro fertilization, or IVF, is a term you might have heard tossed around on TV shows, in magazines, or maybe even in conversations with friends. It’s one of those things that sounds complicated—and honestly, it kind of is—but it’s also a lifeline for millions of people dreaming of starting a family. If you’re curious about what IVF really is, how it works, and whether it might be an option for you or someone you love, you’re in the right place. This article is your go-to guide, breaking it all down in a way that’s easy to grasp, with some fresh insights you won’t find everywhere else.
IVF isn’t just a medical procedure; it’s a journey. It’s about hope, science, and sometimes a little bit of patience. Whether you’re dealing with infertility, exploring options as a single parent, or just want to know more, let’s dive into the world of IVF together.
The Basics: What Does IVF Mean?
IVF stands for “in vitro fertilization.” The phrase “in vitro” is Latin for “in glass,” which gives you a clue about what’s happening: eggs and sperm meet outside the body, usually in a lab dish. Fertilization happens there, and then the resulting embryo (a fertilized egg) is placed into the uterus to grow into a baby. Simple, right? Well, not quite—it’s a multi-step process that involves a mix of hormones, careful timing, and skilled doctors.
Think of IVF like a recipe. You need the right ingredients (eggs and sperm), a perfect environment (the lab), and a skilled chef (your fertility team) to make it all come together. It’s been around since 1978, when the first “test-tube baby,” Louise Brown, was born in England. Since then, over 8 million babies worldwide have come into the world thanks to IVF. That’s a lot of happy parents!
Why Do People Turn to IVF?
IVF isn’t something people jump into without a reason. It’s usually a solution for folks facing challenges that make getting pregnant naturally tough or impossible. Here are some common reasons people choose IVF:
- Blocked or Damaged Fallopian Tubes: These tubes are like highways for eggs to travel from the ovaries to the uterus. If they’re blocked, the egg can’t make the trip.
- Low Sperm Count or Quality: For guys, if the sperm aren’t strong swimmers or there aren’t enough of them, fertilization can be tricky.
- Ovulation Issues: If the ovaries aren’t releasing eggs regularly, there’s nothing for sperm to meet.
- Endometriosis: This condition can mess with the reproductive system, making it harder for eggs and sperm to do their thing.
- Age: As women get older, egg quality and quantity drop, especially after 35. IVF can help by using donor eggs or boosting the process.
- Unexplained Infertility: Sometimes, doctors can’t pinpoint why pregnancy isn’t happening. IVF steps in as a workaround.
- Single Parents or Same-Sex Couples: IVF opens doors for people who want kids without a traditional partner setup, often using donor eggs, sperm, or surrogates.
It’s not just about fixing a problem—it’s about creating possibilities. For example, a single woman in her 30s might freeze her eggs now and use IVF later when she’s ready. Or a couple might use it to avoid passing on a genetic condition. IVF adapts to all kinds of stories.
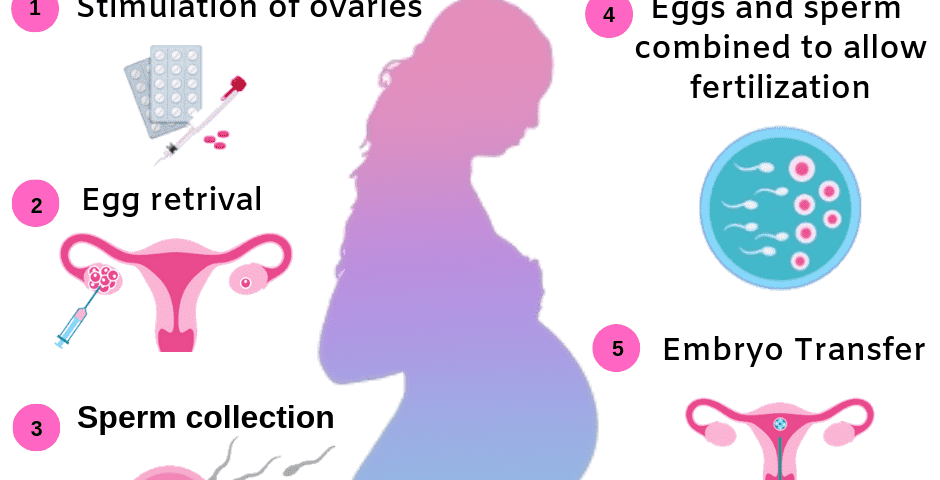
How Does IVF Work? A Step-by-Step Breakdown
IVF isn’t a one-and-done deal. It’s a series of steps that can take weeks or even months. Here’s how it usually goes, explained like a roadmap:
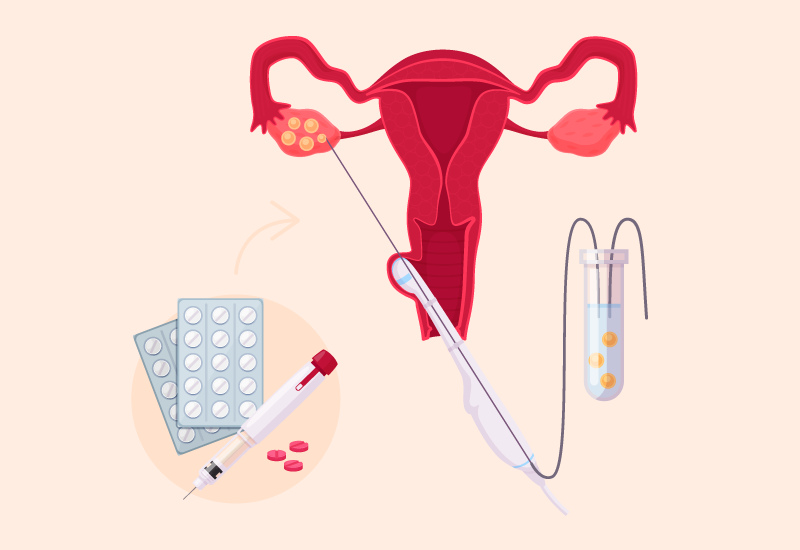
Step 1: Boosting Egg Production
Your ovaries naturally release one egg a month, but IVF needs more to increase the odds of success. You’ll take hormone shots or pills for about 10-14 days to stimulate your ovaries. These meds tell your body, “Hey, let’s make a bunch of eggs!” Doctors keep an eye on things with ultrasounds and blood tests to see how many eggs are growing.
- What to Expect: Mild bloating or mood swings from the hormones. It’s like PMS, but with a purpose.
- Fun Fact: A typical cycle might produce 10-15 eggs, though not all will be usable.
Step 2: Egg Retrieval
Once the eggs are ready, it’s time to get them out. This is a quick procedure (about 20-30 minutes) done under light sedation. A doctor uses a thin needle guided by ultrasound to pull the eggs from your ovaries through your vagina. No big cuts—just a tiny poke.
- Comfort Tip: You’ll rest afterward, but most people are back to normal the next day.
- Reality Check: You might get 8-12 eggs, but some might not mature enough for the next step.
Step 3: Sperm Collection
On the same day, the sperm comes into play. If it’s from a partner, they’ll provide a sample (yep, in that little room at the clinic). If it’s donor sperm, it’s thawed and ready to go. The lab cleans it up, picking the healthiest swimmers.
- Pro Tip: Guys, skip the coffee and tight pants beforehand—sperm like it cool and calm.
Step 4: Fertilization in the Lab
Here’s where the “in vitro” part happens. The eggs and sperm are mixed in a dish. Sometimes, if the sperm need help, doctors use a technique called ICSI (intracytoplasmic sperm injection), where they inject a single sperm right into an egg. After a day or two, you’ve got embryos!
- Success Stat: About 60-70% of eggs fertilize, depending on quality.
Step 5: Embryo Transfer
A few days later (usually 3-5), the best embryo—or two—is placed into the uterus using a thin tube through the cervix. No anesthesia needed—it’s like a Pap smear but with a happier goal. Then, you wait about two weeks to see if it sticks.
- Hopeful Note: If it works, you’re pregnant! If not, you can try again with frozen embryos.
Step 6: The Waiting Game
This is the hardest part: the two-week wait. You might take progesterone (a hormone) to help the embryo settle in. Then, a blood test confirms if you’re pregnant.
- Survival Tip: Distractions help—binge a show, bake cookies, anything but Googling symptoms!
What’s the Success Rate of IVF?
Success isn’t guaranteed with IVF, and it depends on a lot of factors like age, health, and even luck. Here’s a quick look at the numbers, based on 2022 data from the CDC:
| Age Group | Live Birth Rate per Cycle |
|---|---|
| Under 35 | 40-50% |
| 35-37 | 30-40% |
| 38-40 | 20-30% |
| Over 40 | 10-15% |
- Younger Women: Under 35, you’ve got the best shot because egg quality is higher.
- Older Women: Over 40, it drops, but using donor eggs can bump it back up to 50% or more.
Each cycle’s a fresh chance, and many people need 2-3 tries. It’s not a sprint—it’s a marathon with a big prize at the end.
The Emotional Side of IVF
IVF isn’t just about needles and labs; it’s an emotional rollercoaster. One day you’re hopeful, the next you’re stressed about results. Studies show up to 40% of women going through IVF experience anxiety or depression. It’s normal to feel that way—it’s a big deal!
- ✔️ Do This: Talk to someone—a friend, a counselor, or an IVF support group. You’re not alone.
- ❌ Don’t Do This: Bottle it up. It’s okay to cry or vent when you need to.
Here’s a little interactive moment: How Are You Feeling Today?
Take a second to check in with yourself. Are you:
A) Excited and hopeful
B) Nervous but curious
C) Overwhelmed and unsure
No wrong answers—just a way to connect with where you’re at.
Costs and Coverage: What’s the Price Tag?
IVF isn’t cheap. In the U.S., one cycle can run $12,000 to $20,000, not counting meds (another $3,000-$5,000). Insurance coverage varies wildly—some states like New York mandate partial coverage, but most don’t. Globally, places like the UK offer some free cycles through the NHS, while others leave it all out-of-pocket.
- Money-Saving Hack: Look into clinics with package deals (3 cycles for a discount) or financing plans.
- New Trend: Some employers, like Starbucks or Google, now offer IVF benefits. Check your job perks!
Here’s a mini breakdown:
| Expense | Average Cost |
|---|---|
| IVF Cycle | $12,000-$15,000 |
| Medications | $3,000-$5,000 |
| Embryo Freezing | $1,000-$2,000 |
| Genetic Testing | $2,000-$4,000 |
Risks and Side Effects: What to Watch For
IVF is safe overall, but it’s not risk-free. The hormone shots can cause bloating, headaches, or a rare condition called ovarian hyperstimulation syndrome (OHSS), where your ovaries overreact. About 1-2% of women get OHSS, and it’s usually mild.
- Pregnancy Risks: IVF slightly raises the chance of twins (20-30% of pregnancies) or ectopic pregnancy (1-2%).
- Long-Term: No solid evidence links IVF to cancer, despite old worries. A 2023 study in Fertility and Sterility found no increased risk after 20 years.
- ✔️ Watch For: Severe pain or swelling—call your doctor ASAP.
- ❌ Don’t Ignore: Mood swings that feel out of control. Help’s available.
Fresh Insights: What’s New in IVF?
Most articles stick to the basics, but let’s go deeper with some cutting-edge stuff that’s shaking up IVF in 2025:
1. Time-Lapse Imaging
Labs now use cameras to watch embryos grow 24/7. This tech picks the strongest ones without disturbing them. A 2024 study in Human Reproduction showed it boosts success rates by 10-15%. It’s like giving embryos a reality TV audition—only the stars make it to transfer!
2. AI-Powered Embryo Selection
Artificial intelligence is stepping in to analyze embryos. It looks at patterns humans might miss, predicting which ones are most likely to implant. Early trials suggest AI could cut failed cycles by 20%. Imagine a super-smart assistant helping your doctor—it’s here!
3. Mini-IVF: Less Is More
Traditional IVF uses heavy hormone doses, but “mini-IVF” goes lighter, aiming for fewer, higher-quality eggs. It’s cheaper (around $5,000-$7,000) and easier on your body. A 2023 pilot study found similar success rates for women under 35. It’s like a low-key version of the classic recipe.
IVF Myths Busted
There’s a lot of noise out there about IVF. Let’s clear up some myths with facts:
- Myth: IVF babies are “unnatural.”
Truth: They’re as natural as any baby—just conceived in a dish instead of a body. They grow in the uterus like everyone else. - Myth: IVF always means twins.
Truth: Single transfers are now standard to avoid multiples. Twins happen, but it’s not the goal. - Myth: It’s only for rich people.
Truth: Costs are high, but grants, loans, and global options (like clinics in Mexico for $6,000) make it more accessible.
Real Stories: IVF in Action
Numbers and steps are great, but stories bring it home. Meet Sarah, a 38-year-old teacher from Ohio. After three years of trying naturally, she and her husband turned to IVF. “The shots were rough,” she says, “but seeing that first ultrasound made it worth it.” Their son, Liam, just turned two. Sarah’s tip? “Find a clinic that feels like family—they’ll get you through the lows.”
Then there’s James, a single dad in California. At 42, he used IVF with donor eggs and a surrogate. “I didn’t want to wait for ‘the one’ to have a kid,” he explains. His daughter, Mia, arrived last year. James says the process taught him patience—and how to advocate for himself with doctors.
Your IVF Prep Checklist
Thinking about IVF? Here’s a practical list to get ready:
- ✔️ Research Clinics: Look for high success rates and good reviews. Ask about their embryo lab—top-notch equipment matters.
- ✔️ Check Finances: Call your insurance and explore grants like Baby Quest Foundation.
- ✔️ Boost Health: Eat well, cut stress, and skip alcohol. A 2024 study linked a Mediterranean diet to better IVF outcomes.
- ✔️ Ask Questions: Write down everything—how many embryos? What’s the timeline? No question’s too small.
- ❌ Don’t Rush: Take time to feel sure. It’s a big step, not a race.
The Future of IVF: Where Are We Headed?
IVF’s evolving fast. Beyond AI and mini-IVF, scientists are exploring:
- Ovarian Tissue Freezing: For cancer patients, freezing ovary slices could preserve fertility long-term. A 2025 trial in Europe showed promise with three live births.
- Lab-Grown Eggs: Researchers are trying to make eggs from stem cells. It’s years away, but it could rewrite the rules for older women or those with no eggs left.
- Affordable Access: Advocacy groups are pushing for more insurance coverage and lower costs. By 2030, experts predict IVF could drop to $5,000 per cycle with new tech.
Interactive Quiz: Is IVF Right for You?
Let’s make this fun! Answer these quick questions (in your head or on paper) to see where you stand:
- Are you under 40 and struggling to conceive after a year?
- Yes / No
- Do you have a condition like endometriosis or low sperm count?
- Yes / No
- Are you open to medical help to build your family?
- Yes / No
- Can you handle a process that might take a few months?
- Yes / No
If you’ve got mostly “Yes” answers, IVF might be worth exploring with a doctor. No pressure—just a starting point!
Three Things You Haven’t Heard About IVF
Most articles skip these nuggets, but they’re game-changers:
1. The Sperm Factor No One Talks About
Sperm DNA damage is a hidden hurdle. A 2024 study in Andrology found that men over 40 often have more fragmented sperm DNA, lowering IVF success. Clinics can test for this now and tweak treatments—like using antioxidants or ICSI—to improve odds. Ask your doctor about it; it’s not routine yet.
2. Your Gut Matters
Your microbiome (the bacteria in your gut) might affect IVF. A small 2023 study linked a balanced gut to higher implantation rates. Probiotics or a diet rich in yogurt and fiber could give you an edge. It’s early research, but it’s a low-risk boost to try.
3. The Frozen Advantage
Frozen embryo transfers (FET) are outpacing fresh ones. Why? They let your body recover from hormones before implantation, upping success by 5-10%, per a 2025 Fertility Journal report. Plus, you can time it better. Fresh transfers are still common, but FET’s the quiet star.
Tips for the IVF Journey
Here’s some real-world advice to make it smoother:
- Build a Support Crew: Tell a few trusted people—your mom, best friend, or even an online group. They’ll cheer you on.
- Track Everything: Use an app or notebook for meds, appointments, and feelings. It keeps chaos at bay.
- Celebrate Small Wins: Got through egg retrieval? Treat yourself to ice cream. Every step counts.
- Plan for Downtime: The two-week wait is brutal—stock up on books, movies, or a craft project.
Wrapping It Up: IVF Is Your Story
IVF isn’t just science—it’s personal. It’s about taking control when nature throws a curveball. Whether you’re dreaming of a baby now or banking eggs for later, it’s a path paved with resilience and hope. Sure, it’s got challenges—costs, emotions, waiting—but it’s also got millions of success stories.
So, what’s next? If IVF’s on your radar, talk to a fertility specialist. Ask about your odds, costs, and what feels right for you. It’s not a one-size-fits-all deal—it’s your journey, your way. And who knows? Maybe this is the start of something amazing.