What’s IVF? Your Complete Guide to In Vitro Fertilization
April 16, 2025
What Does IVF Mean? Your Complete Guide to Understanding In Vitro Fertilization
April 16, 2025What Does IVF Stand For? Your Complete Guide to In Vitro Fertilization
If you’ve ever wondered what IVF stands for, you’re not alone. It’s a term that pops up a lot these days, especially for people dreaming of starting a family but facing some roadblocks. IVF stands for In Vitro Fertilization, a process where an egg and sperm are combined outside the body to create an embryo, which is then placed in the uterus to grow into a baby. Simple, right? Well, not quite—there’s so much more to it than that! Whether you’re curious about how it works, who it’s for, or what the latest science says, this guide has you covered with everything you need to know.
IVF isn’t just a medical procedure; it’s a lifeline for millions of people. Since the first IVF baby, Louise Brown, was born in 1978, over 12 million babies worldwide have come into the world thanks to this technology. But even with all that success, IVF can feel like a mystery. Let’s break it down step-by-step, sprinkle in some real-life insights, and explore angles you might not find in the usual articles—like how your lifestyle impacts success or what’s new in 2025 research.
What Is IVF, Exactly?
In Vitro Fertilization—IVF for short—is a type of assisted reproductive technology (ART). The phrase “in vitro” comes from Latin, meaning “in glass,” because the magic happens in a lab dish, not inside the body. Picture this: doctors take eggs from the ovaries, mix them with sperm in a controlled environment, and then transfer the resulting embryo into the uterus. If all goes well, that embryo implants and grows into a baby.
It’s different from natural conception, where the egg and sperm meet in the fallopian tube. IVF steps in when that natural process isn’t working, whether due to blocked tubes, low sperm count, or other challenges. Think of it like giving nature a little nudge with some high-tech help.
How Did IVF Start?
The story of IVF kicked off with a groundbreaking moment in 1978 when Louise Brown was born in England. Scientists Patrick Steptoe and Robert Edwards spent years perfecting the technique, and their work earned Edwards a Nobel Prize in 2010. Back then, it was called the “test-tube baby” method—a nickname that stuck even though it’s done in petri dishes, not test tubes. Today, IVF has evolved into a polished process, helping people of all ages and backgrounds build families.

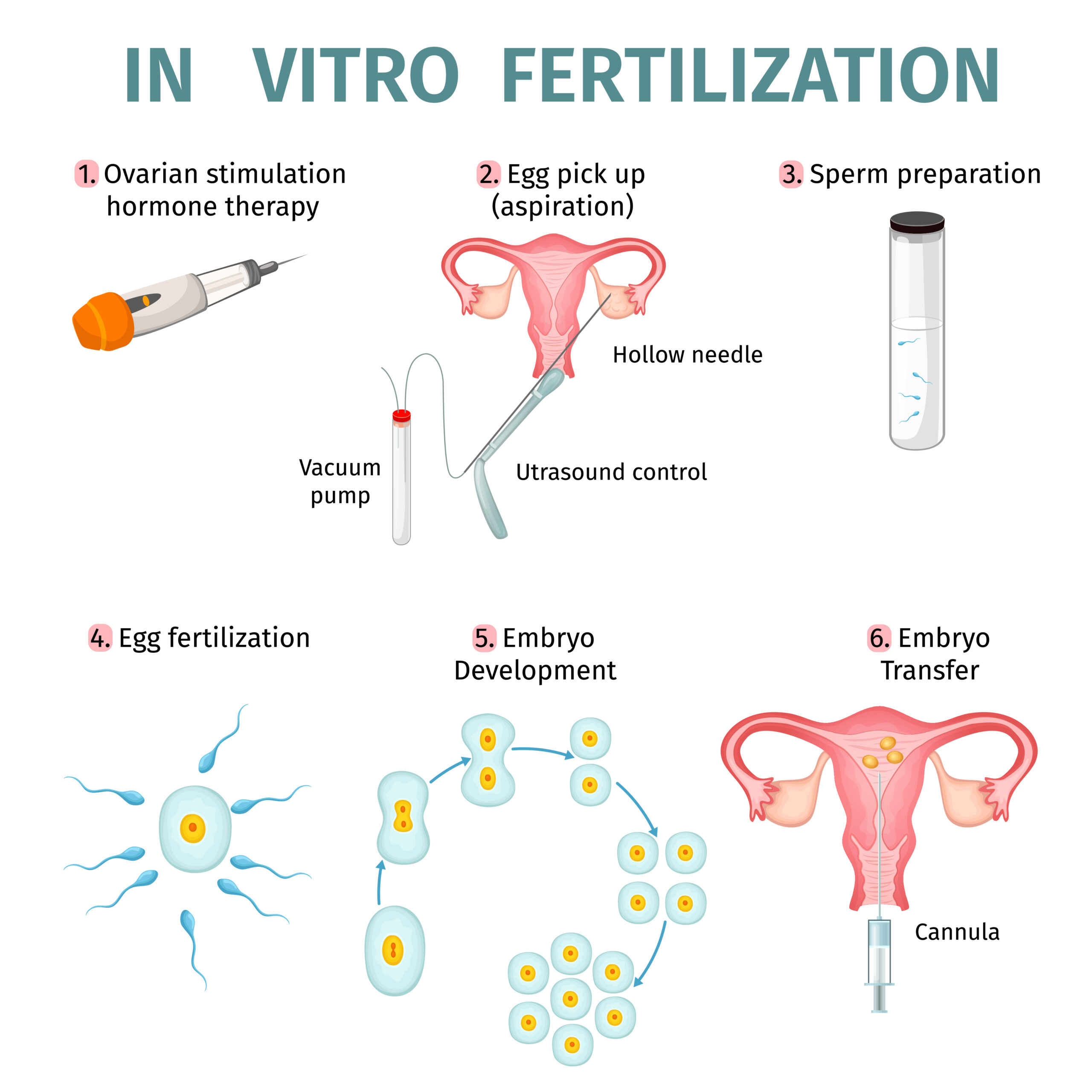
How Does IVF Work? A Step-by-Step Breakdown
IVF isn’t a one-and-done deal—it’s a journey with several stages. Here’s what happens, explained in a way that’s easy to follow:
Step 1: Boosting Egg Production
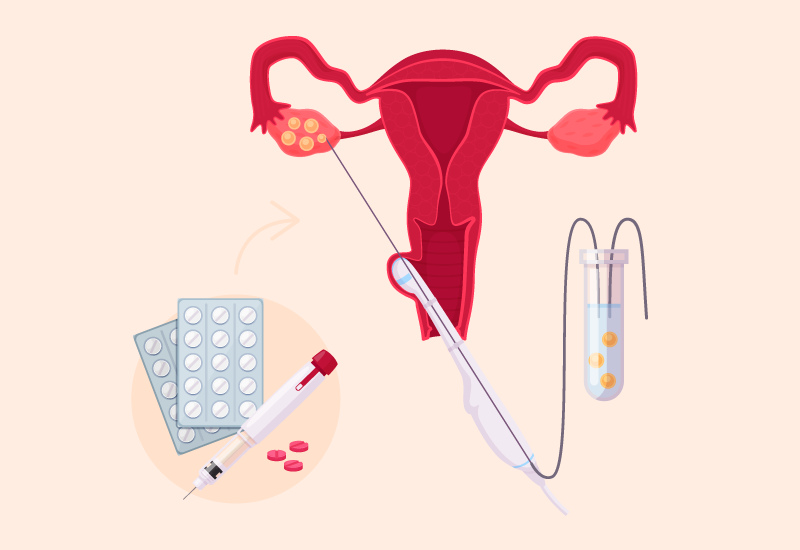
First, a woman takes fertility drugs to encourage her ovaries to produce multiple eggs. Normally, your body releases one egg a month, but IVF needs more to increase the odds of success. These meds—like follicle-stimulating hormone (FSH)—are usually injections you give yourself at home. Doctors monitor your progress with ultrasounds and blood tests to see how those eggs are growing.
✔️ Tip: Keep a small journal to track your shots and appointments—it helps you feel in control!
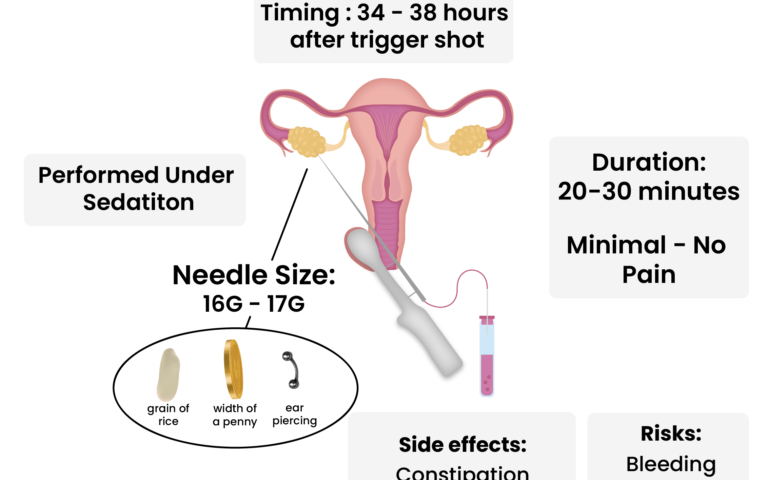
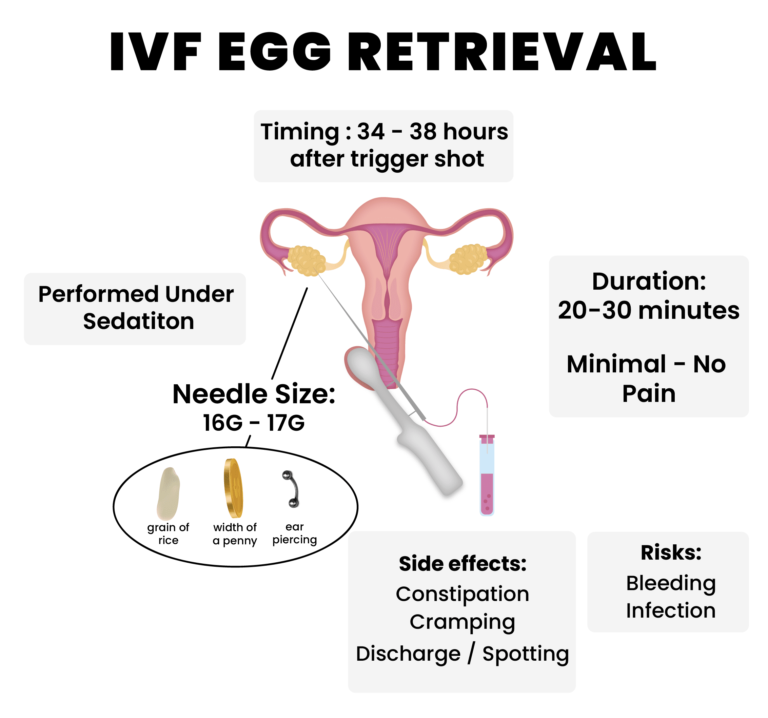
Step 2: Egg Retrieval
Once the eggs are ready (about 10-14 days later), it’s time to collect them. This minor surgery, called egg retrieval, happens under light sedation. A doctor uses a thin needle guided by ultrasound to pull the eggs from your ovaries. It takes about 20-30 minutes, and you’ll rest for a bit afterward.
❌ Don’t worry: It’s not as scary as it sounds—most people say it’s like a quick nap with some mild cramping after.
Step 3: Fertilization in the Lab
Next, the eggs meet the sperm in the lab. There are two ways this can happen:
- Traditional IVF: Eggs and sperm are mixed together in a dish, letting nature take its course.
- ICSI (Intracytoplasmic Sperm Injection): A single sperm is injected directly into an egg, often used if sperm quality is low.
The fertilized eggs—now embryos—grow for 3-5 days under the watchful eye of embryologists.
Step 4: Embryo Transfer
A few days later, one or two healthy embryos are placed into the uterus using a thin catheter. It’s a quick, painless procedure—no anesthesia needed. If the embryo implants in the uterine lining, pregnancy begins. Extra embryos can be frozen for later use.
Step 5: The Waiting Game
About 10-14 days after the transfer, you take a pregnancy test. This two-week wait can feel endless, but it’s when the embryo decides if it’s sticking around.
Who Can Benefit from IVF?
IVF isn’t just for one type of person—it’s a tool for all kinds of fertility struggles. Here’s who might turn to it:
- Women with blocked or damaged fallopian tubes: If the tubes are out of commission, eggs can’t meet sperm naturally.
- Men with low sperm count or motility: IVF (especially ICSI) can work with just a few good swimmers.
- Couples with unexplained infertility: When doctors can’t pinpoint the issue, IVF often steps in.
- Older women: As egg quality drops with age, IVF can use donor eggs or boost chances with multiple embryos.
- Same-sex couples or single parents: Using donor eggs, sperm, or surrogates, IVF opens doors to parenthood.
- People preserving fertility: Cancer patients or those delaying kids can freeze eggs or embryos for later.
In 2021, the CDC reported that 2.5% of U.S. babies were born via IVF. That’s a lot of families who might not exist without it!
What Are the Success Rates?
Success isn’t guaranteed with IVF, but the numbers are encouraging—and they’re getting better. Here’s a snapshot based on 2021 data from the Society for Assisted Reproductive Technology (SART):
| Age Group | Live Birth Rate per Cycle |
|---|---|
| Under 35 | 50.8% |
| 35-37 | 32.4% |
| 38-40 | 20.1% |
| 41-42 | 9.7% |
| Over 42 | 2.9% |
What Boosts Your Odds?
- Younger age: More eggs, better quality.
- Previous pregnancy: Shows your body can carry a baby.
- Single embryo transfer: Reduces risks and focuses on the strongest embryo.
- Healthy lifestyle: More on this later—it’s a game-changer!
The catch? These are averages. Your personal odds depend on your health, the clinic’s expertise, and even a bit of luck.
What’s It Like to Go Through IVF?
IVF is a rollercoaster—physically, emotionally, and financially. Let’s walk through what you might experience.
The Physical Side
- Injections: Daily shots for 1-2 weeks. They sting a little, but you get the hang of it.
- Egg Retrieval: Mild bloating or cramping for a day or two.
- Transfer: Feels like a Pap smear—quick and easy.
- Side Effects: Hormones can bring mood swings, fatigue, or bloating. A rare risk is ovarian hyperstimulation syndrome (OHSS), where ovaries overreact, but it’s manageable with care.
The Emotional Ride
One minute you’re hopeful, the next you’re anxious. The two-week wait is the toughest part—every twinge feels like a clue. Having a support system, like a partner or friend, makes a huge difference.
The Cost
IVF isn’t cheap. In the U.S., one cycle averages $15,000-$25,000, including meds. Insurance coverage varies—some states mandate it, but many don’t. Freezing embryos or doing extra cycles adds to the bill.
✔️ Money-Saving Tip: Look into fertility grants or clinics with payment plans. Every little bit helps.
Interactive Quiz: Is IVF Right for You?
Take a quick moment to think about your situation with this mini-quiz. Answer yes or no:
- Have you been trying to conceive for over a year (or 6 months if over 35)?
- Do you or your partner have a known fertility issue (like low sperm count or endometriosis)?
- Are you open to medical procedures and a few weeks of treatment?
If you said yes to any of these, IVF might be worth exploring with a doctor. It’s not a commitment—just a starting point!
The Risks and Realities of IVF
IVF is safe overall, but it’s not risk-free. Here’s what to watch for:
- Multiple Pregnancies: Transferring more than one embryo can lead to twins or triplets, raising risks like preterm birth.
- Ectopic Pregnancy: Rarely, the embryo implants outside the uterus (about 2-5% of cases).
- OHSS: Affects 1-5% of patients, causing bloating or pain, but severe cases are uncommon.
- Emotional Toll: Failed cycles can hit hard. Counseling or support groups can be a lifeline.
The good news? Advances in 2025—like better embryo screening—keep reducing these risks.
How Your Lifestyle Impacts IVF Success
Here’s something you won’t find in every IVF article: your daily habits matter more than you think. Research backs this up, and it’s an area where you have real power.
What Helps
- Eat Smart: A Mediterranean diet (think fish, veggies, olive oil) boosts egg quality, per a 2023 study in Fertility and Sterility. Women who ate this way had a 20% higher success rate.
- Move More: Moderate exercise—like 30 minutes of walking 5 days a week—improves blood flow to reproductive organs.
- Sleep Well: Aim for 7-8 hours. Poor sleep messes with hormones, lowering your odds.
What Hurts
- Smoking: Cuts success rates by up to 50%, says the American Society for Reproductive Medicine (ASRM).
- Too Much Caffeine: Over 300 mg daily (about 3 cups of coffee) may reduce implantation chances.
- Stress: Chronic stress raises cortisol, which can disrupt embryo development.
✔️ Action Step: Try a 10-minute mindfulness session daily—apps like Calm make it easy.
What’s New in IVF for 2025?
IVF isn’t standing still. Here are three cutting-edge updates you won’t see everywhere:
1. AI-Powered Embryo Selection
Clinics now use artificial intelligence to pick the best embryos. A 2024 study from Stanford showed AI boosts success rates by 15% by analyzing embryo images faster and more accurately than humans.
2. Microfluidics for Sperm Sorting
This tech uses tiny channels to select the healthiest sperm, improving fertilization rates. It’s like a high-tech filter, and early trials in 2025 show promise for couples with male infertility.
3. Stem Cell Gametes
Scientists are working on turning stem cells into eggs or sperm. A 2023 breakthrough in Japan created viable mouse sperm this way—human trials are next. This could help people with no viable gametes have biological kids.
These advances mean IVF is getting smarter, safer, and more accessible every year.
IVF Myths vs. Facts
There’s a lot of noise out there about IVF. Let’s clear up some common misconceptions:
- Myth: IVF babies have more birth defects.
- Fact: The risk is slightly higher (4% vs. 3% naturally), but it’s often tied to infertility itself, not IVF, per the CDC.
- Myth: IVF is only for women.
- Fact: It helps men with sperm issues too—ICSI is a game-changer.
- Myth: IVF always works on the first try.
- Fact: Most people need 2-3 cycles for success, depending on age and health.
Real Stories: IVF in Action
Meet Sarah, a 38-year-old teacher from California. After two years of trying naturally, she and her husband turned to IVF due to endometriosis. “The shots were tough, but seeing our embryo on the screen made it real,” she says. Their first cycle worked, and their son is now 2. Sarah’s tip? “Trust your team, but ask questions—it’s your journey.”
Then there’s James, a single dad in Texas. Using a donor egg and surrogate, he welcomed twins in 2024. “IVF gave me a family I never thought possible,” he shares. His advice: “Plan financially—it’s worth every penny.”
These stories show IVF’s power—and its personal side.
Interactive Checklist: Preparing for IVF
Ready to take the plunge? Use this checklist to get started:
- ✔️ Talk to a fertility specialist (ask about success rates and costs).
- ✔️ Get a full health check—hormones, sperm count, the works.
- ✔️ Cut back on smoking, alcohol, and stress triggers.
- ✔️ Save up or research funding options.
- ✔️ Build a support crew—friends, family, or a therapist.
Tick these off, and you’re on your way!
Three Things You Haven’t Heard About IVF
Most articles stick to the basics, but here are three under-the-radar topics that deserve more attention:
1. The Role of Gut Health
A 2024 study in Nature Reproductive Medicine found that a balanced gut microbiome improves IVF outcomes. Women with higher levels of good bacteria (like Lactobacillus) had a 25% better implantation rate. Probiotics might be your secret weapon—talk to your doctor about adding them.
2. Mental Prep Is as Important as Physical
Everyone focuses on the body, but your mind needs TLC too. A 2023 survey of 500 IVF patients showed 70% felt unprepared for the emotional ups and downs. Try journaling or a support group—it’s not just fluff; it keeps you grounded.
3. The Frozen Embryo Debate
Freezing embryos is standard, but what happens if you don’t use them? Some donate to research, others to other couples, but legal battles—like Alabama’s 2024 ruling calling embryos “children”—are shaking things up. It’s a personal choice with big implications.
How to Choose an IVF Clinic
Not all clinics are equal. Here’s what to look for:
- Success Rates: Check SART or CDC data—aim for above-average numbers for your age group.
- Experience: How long have they been doing IVF? More years often mean more skill.
- Tech: Do they offer AI screening or genetic testing?
- Vibes: Visit the clinic—do you feel heard and cared for?
✔️ Pro Tip: Ask how many cycles they recommend before switching strategies. A good clinic tailors the plan to you.
IVF Around the World
IVF isn’t the same everywhere. In Japan, cherry blossom season 2025 sparked posts on X about couples timing IVF with nature’s renewal—a cultural twist you won’t see in the U.S. In Europe, countries like Denmark cover up to three cycles for free, while the U.S. leaves most to pay out of pocket. These differences shape how people experience IVF globally.
Your Next Steps
IVF might feel overwhelming, but it’s a path millions have walked. Start by talking to your doctor or a fertility specialist—they’ll map out what’s possible for you. Read up, ask questions, and lean on your crew. Whether it’s your first step or your next, you’re not alone in this.
What’s your biggest IVF question? Drop it in the comments—I’d love to hear from you! And if you’ve been through it, share your story. It might just light the way for someone else.