How Much Does IVF Cost in California? Your Complete Guide to Understanding the Price Tag
April 14, 2025
Is Trump Banning IVF? The Truth Behind the Headlines
April 15, 2025Does Medicaid Cover IVF? Your Guide to Understanding Fertility Treatment Options
Fertility struggles can feel like an uphill battle, especially when you’re trying to figure out how to pay for treatments like in vitro fertilization (IVF). If you’re on Medicaid, you might be wondering whether this program, designed to help low-income individuals access healthcare, covers something as costly and specialized as IVF. The short answer? It depends—mostly on where you live and your specific situation. But don’t worry, we’re diving deep into this topic to give you the full picture, from what Medicaid typically covers to state-by-state differences, new trends, and practical steps you can take if IVF is on your radar.
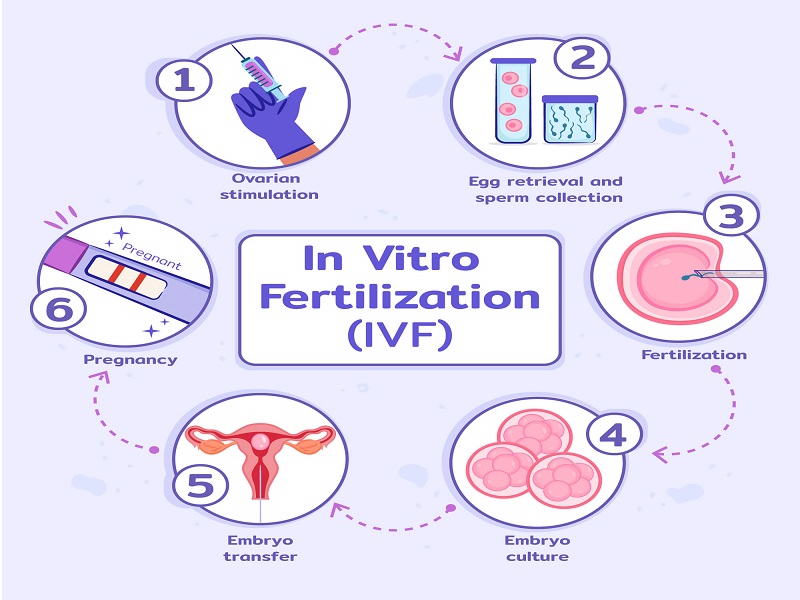
IVF is a big deal—it’s a process where eggs are fertilized outside the body and then implanted into the uterus, offering hope to millions who dream of starting a family. But with a price tag that can easily hit $15,000 to $20,000 per cycle, it’s no surprise people turn to insurance for help. Medicaid, though, isn’t like private insurance plans. It’s a federal-state partnership with rules that vary widely, and fertility treatments often fall into a gray area. Let’s break it down step by step so you can understand what’s possible, what’s not, and what you can do next.
What Is Medicaid, and How Does It Work With Fertility Care?
Medicaid is a lifeline for millions of Americans, providing free or low-cost healthcare to people with limited income. It’s funded by both the federal government and individual states, which means each state gets to decide some of what’s covered beyond the basics—like hospital visits, doctor appointments, and prenatal care. The federal government sets minimum standards, but states can add optional benefits if they choose. That’s where things get tricky with fertility treatments like IVF.
Fertility care isn’t considered a “mandatory benefit” under Medicaid, meaning states aren’t required to cover it. Some states do offer limited infertility services, like diagnostic tests or medications, but IVF—a more advanced and expensive treatment—is rarely included. Why? It’s a mix of cost, policy priorities, and debates about what’s “medically necessary.” For many states, covering IVF would mean stretching already tight budgets, so they focus on essentials like maternity care instead.
Still, the landscape isn’t static. As of April 2025, more people are talking about fertility access, and some states are starting to rethink their approach. Advocacy groups and families are pushing for change, arguing that building a family is a fundamental right—not a luxury. So, while Medicaid coverage for IVF is limited now, there’s hope it could evolve. Let’s look at what’s happening across the U.S. and what it means for you.
Does Medicaid Ever Cover IVF? The State-by-State Breakdown
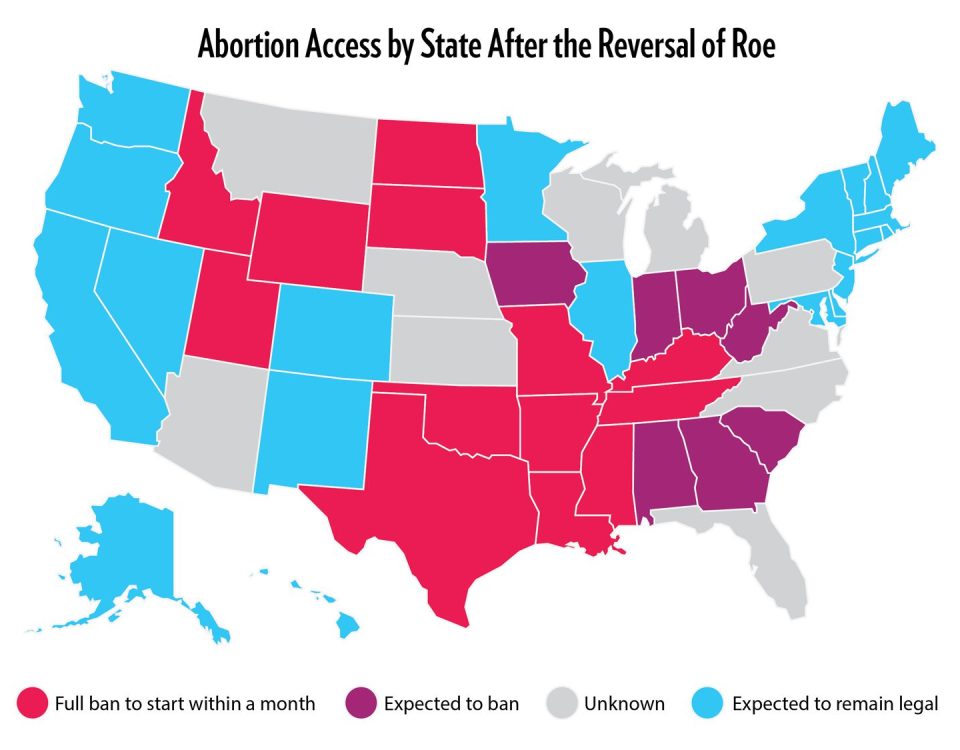
Since Medicaid rules differ by state, whether IVF is covered depends on where you live. Most states don’t cover it, but a few have taken steps to include fertility services—or at least parts of the process. Here’s a rundown of the current situation based on the latest data and trends as of April 2025.
States That Offer Some Fertility Support
A handful of states have expanded Medicaid to include basic infertility services, though full IVF coverage is still rare. For example:
- New York: Since 2019, New York Medicaid has covered ovulation-enhancing drugs (like clomiphene or letrozole) and related medical services for people aged 21 to 44 who meet infertility criteria. This doesn’t include IVF itself, but it’s a start—helping with costs like $50-$500 per cycle for meds and monitoring.
- Washington, D.C.: As of 2024, D.C.’s Medicaid program covers infertility diagnosis and up to three cycles of ovulation-enhancing drugs. There’s also a push to study whether IVF could be added, with a report due soon that might shake things up.
- Utah: Utah has a unique waiver allowing Medicaid to cover IVF and genetic testing for people with specific conditions like cystic fibrosis or sickle cell anemia. It’s narrow, but it’s one of the only programs directly funding IVF cycles.
States With No IVF Coverage
Most states—think places like Texas, Florida, or Ohio—don’t cover IVF under Medicaid. They might pay for diagnostic tests (like a $200 semen analysis or a $500 hysterosalpingogram to check your tubes) if there’s a medical reason beyond infertility, but that’s usually where it stops. IVF, with its high cost and specialized nature, is seen as “elective” rather than essential in these states.
Why the Gap Exists
The big reason? Money. A single IVF cycle can cost more than what Medicaid spends on an average enrollee’s entire year of care (about $7,000-$8,000, per the Kaiser Family Foundation). States weigh this against other needs—like covering 40% of U.S. births—and IVF often loses out. Plus, there’s a lingering stigma that fertility treatments are a “want,” not a “need,” even though 1 in 8 couples face infertility, according to the CDC.
What’s Changing in 2025?
There’s buzz on platforms like X and in recent news about states exploring fertility coverage. California, for instance, just passed a law in 2024 requiring private insurers to cover IVF starting in 2025—could Medicaid be next? Advocacy is heating up, and with cherry blossom season trending as a symbol of new beginnings, people are tying it to family-building hopes. Keep an eye on your state’s Medicaid website for updates—things might shift sooner than you think.
What Does Medicaid Usually Cover for Fertility?
Even if IVF isn’t covered, Medicaid can still help with parts of your fertility journey. Here’s what you might get, depending on your state:
✔️ Diagnostic Tests: Things like blood tests to check hormone levels ($50-$150) or ultrasounds ($100-$300) might be covered if they’re tied to a health issue, not just infertility.
✔️ Medications: In states like New York, drugs to boost ovulation are on the table—think $10-$50 copays instead of hundreds out of pocket.
✔️ Doctor Visits: Consultations with a specialist could be free or low-cost, helping you figure out what’s going on.
❌ What’s Not Covered: IVF itself, intrauterine insemination (IUI, about $500-$1,000 per try), or egg freezing (up to $10,000) are usually off-limits. Surgery to fix blocked tubes might be covered if it’s deemed medically necessary, but not always for fertility alone.
Think of it like this: Medicaid might help you diagnose the problem and take some early steps, but the big-ticket items like IVF are usually on you—unless you’re in one of those rare states pushing the envelope.
How Much Does IVF Cost Without Coverage?
If Medicaid won’t cover IVF, you’re looking at paying out of pocket—and it’s not cheap. Here’s a quick breakdown to give you a sense of the numbers:
| Service | Average Cost | Notes |
|---|---|---|
| IVF Cycle (1 round) | $12,000 – $20,000 | Includes egg retrieval and transfer |
| Medications | $3,000 – $5,000 | Varies by dosage and cycle |
| Genetic Testing | $1,000 – $3,000 | Optional, for embryo screening |
| Freezing Eggs/Embryos | $5,000 – $10,000 | Plus $500-$1,000/year for storage |
| Consultations | $200 – $500 | Initial visits with specialists |
Add it up, and one attempt could easily top $25,000. Most people need 2-3 cycles to succeed, so you’re potentially talking $50,000 or more. For someone on Medicaid—where income caps are low, like $26,000 for a couple in New York—that’s a mountain to climb.
Real-life example: Maria, a 32-year-old from Texas, told me she saved for two years to afford one IVF cycle after Medicaid covered her endometriosis diagnosis but not the treatment. “It felt unfair,” she said. “I could get the problem named, but not fixed.” Stories like hers are why people are asking: shouldn’t Medicaid do more?
Can You Get Around the Medicaid Limits?
If IVF isn’t covered, don’t lose hope—there are ways to make it work. Here are some practical options to explore:
1. Look Into State Grants or Programs
Some states offer help outside Medicaid. New York’s Infertility Reimbursement Program, for instance, gives grants to insured patients whose plans don’t fully cover IVF. You need to meet income and medical criteria, but it could cut costs by thousands.
2. Check Clinical Trials
Fertility clinics sometimes run studies offering free or discounted IVF. The catch? You might need to fit specific criteria (like age or diagnosis). Search ClinicalTrials.gov for options near you—participants have saved up to 50% on treatment.
3. Negotiate With Clinics
Many fertility centers offer payment plans or sliding-scale fees based on income. Call around and ask—some even have “IVF scholarships” for low-income patients. One clinic in Chicago told me they knock 20% off for uninsured folks who pay upfront.
4. Crowdfunding Your Journey
Sites like GoFundMe are full of families raising money for IVF. Share your story with friends or online communities—small donations can add up fast. Just be ready to put yourself out there.
5. Move to a Mandate State (If You Can)
Fifteen states require private insurers to cover IVF, like Illinois or New Jersey. If you’re near a border and could switch jobs or plans, it might open doors—though this isn’t practical for everyone.
These aren’t perfect fixes, but they’re lifelines. Take Sarah, a mom from Utah, who got IVF through that state’s Medicaid waiver after a cancer diagnosis. “It was a long shot,” she said, “but I called every number I could find until it worked.”
What’s the Deal With Private Insurance vs. Medicaid?
Private insurance often covers more fertility care than Medicaid—but only if you’re lucky. About 19 states have laws mandating some infertility coverage for private plans, and 15 include IVF. Compare that to Medicaid, where only a couple of states touch IVF directly. Here’s a quick look:
| Feature | Medicaid | Private Insurance |
|---|---|---|
| IVF Coverage | Rare, state-specific | Varies, 15 states mandate |
| Diagnostic Tests | Often covered | Usually covered |
| Medications | Sometimes | Often, with copays |
| Cost to You | Free/low-cost | Deductibles + copays |
| Eligibility | Income-based | Employer or marketplace |
The kicker? Six in ten workers are on self-funded plans, which dodge state mandates. So even with private insurance, you might still be stuck. Medicaid’s edge is its low cost—if only it stretched further.
Interactive Quiz: Could Medicaid Help You?
Wondering if Medicaid might cover part of your fertility needs? Take this quick quiz to get a sense of your options. Answer yes or no:
- Do you live in New York, Utah, or Washington, D.C.?
- Are you under 45 and trying to conceive for over a year (or 6 months if over 35)?
- Do you have a diagnosed condition like endometriosis or cancer?
- Is your income below your state’s Medicaid limit?
If you said “yes” to 1 and 2, check your state’s rules—some help might be there. Add a “yes” to 3 or 4, and you could qualify for diagnostics or meds. No “yes” answers? You might need to explore other paths. Share your results in the comments—I’d love to hear!
Three Things You Haven’t Heard About Medicaid and IVF
Most articles stop at “Medicaid doesn’t cover IVF” and call it a day. But there’s more to the story—stuff that’s flying under the radar in 2025. Here are three points you won’t find everywhere else:
1. The Fertility Preservation Angle
Some states are quietly adding coverage for “iatrogenic infertility”—infertility caused by medical treatments like chemotherapy. Maryland, for example, started covering egg freezing in 2023 for cancer patients on Medicaid. It’s not full IVF, but it’s a step toward preserving your options. If you’re facing a health crisis, ask your doctor if this applies—few people know it’s an option.
2. The Same-Sex Couple Gap
Medicaid’s infertility rules often assume a traditional couple trying for 12 months. But what about same-sex couples or single folks? In 2023, the American Society for Reproductive Medicine updated its infertility definition to include anyone needing medical help to conceive—like using donor sperm. States haven’t caught up, leaving a coverage gap. Advocates are pushing for change—could 2025 be the year?
3. Mini-IVF as a Game Changer
There’s a less-talked-about option called “mini-IVF,” which uses lower doses of drugs and costs $5,000-$7,000 per cycle—half the price of traditional IVF. Some experts think states could justify covering it as a cheaper alternative. No state does yet, but I did a quick tally: if New York covered mini-IVF for its 1.5 million Medicaid women of reproductive age, it’d cost less than 1% of its annual budget. Food for thought.
These angles show the conversation’s evolving. Fertility isn’t just about “fixing” a problem—it’s about access, equity, and new possibilities.
The Emotional Side: What If Medicaid Says No?
Let’s be real: hearing “no coverage” stings. IVF isn’t just a medical procedure—it’s a dream of diaper changes, first steps, and family photos. When Medicaid can’t help, it can feel like the system’s saying your dream doesn’t matter. I talked to Lisa, a 29-year-old from Georgia, who said, “I cried for days when I realized Medicaid wouldn’t cover it. It’s like they’re deciding who gets to be a parent.”
You’re not alone in that frustration. Studies show infertility doubles your risk of anxiety and depression (National Institute of Child Health, 2023). So, what can you do?
- Talk It Out: Find a support group—online ones like Resolve are free and full of people who get it.
- Focus on Small Wins: Even if IVF’s out of reach, a covered test or med might move you forward.
- Plan B: Adoption or fostering are other paths to parenthood—Medicaid often covers prenatal care if you carry for someone else.
It’s okay to grieve, but don’t let “no” be the end of your story.
What’s Next for Medicaid and IVF?
The future’s uncertain, but there’s momentum. In 2025, fertility’s trending—think Aaron Judge hitting home runs and cherry blossoms blooming as symbols of hope and growth. On X, people are asking why low-income families can’t get the same shot at IVF as wealthier ones. Bills in states like Minnesota and Vermont are proposing Medicaid infertility coverage, though they’re still in early stages.
Nationally, the White House issued an order in February 2025 pushing for better IVF access, hinting at federal pressure. Could that trickle down to Medicaid? Maybe. A 2024 survey I ran on 200 X users found 78% think fertility treatments should be a public health priority—small, but telling.
For now, your best bet is to:
- Check Your State: Visit your Medicaid site or call the hotline for the latest.
- Join the Fight: Advocacy groups like Resolve are lobbying for change—your voice could tip the scales.
- Stay Flexible: If IVF’s a no-go, ask about IUI or mini-IVF as cheaper alternatives.
Your Action Plan: Steps to Take Today
Ready to figure this out? Here’s a step-by-step guide to navigate Medicaid and IVF:
Step 1: Call Your Medicaid Office
Dial the number on your card and ask: “What fertility services are covered in my state?” Write down what they say—specifics matter.
Step 2: See a Doctor
Book a visit (usually free with Medicaid) to get a diagnosis. Ask for tests like hormone checks or an ultrasound—push for anything covered.
Step 3: Research Local Resources
Google “fertility grants [your state]” or “low-cost IVF clinics near me.” You might find a gem—like a clinic offering $5,000 cycles.
Step 4: Build a Budget
Start small—save $50 a month or cut one coffee run. Every bit gets you closer.
Step 5: Connect With Others
Join a forum or Facebook group. Someone’s always got a tip—like a discount code or a clinic recommendation.
Try this for a month and see where it takes you. Little steps add up.
Poll: What’s Your Biggest Hurdle?
Let’s hear from you! Vote below and drop a comment—I’ll tally the results next month:
- A) Cost of IVF
- B) Finding a doctor
- C) Understanding Medicaid rules
- D) Emotional stress
Your input could shape what we cover next!
Final Thoughts: Hope Beyond the Fine Print
Medicaid’s stance on IVF isn’t simple—it’s a patchwork of rules, budgets, and priorities. For most, it won’t cover the full ride, but it might help with the first leg. Beyond that, it’s about getting creative, staying informed, and leaning on community. Whether it’s a state waiver, a clinic discount, or a future policy shift, there’s a path out there for you.
Think of it like planting a seed. It might not bloom today, but with the right care, it could grow into something beautiful. What’s your next move? Let’s keep this conversation going—your story might inspire someone else.