How Long Does IVF Treatment Take? Your Complete Guide to the Timeline
April 23, 2025
How Much Does IVF Cost with Insurance?
April 23, 2025How Many Follicles Do You Need for IVF Success?
If you’re diving into the world of in vitro fertilization (IVF), you’ve probably heard the term “follicles” thrown around a lot. Maybe you’re wondering what they are, why they matter, or—most importantly—how many you need to make your IVF journey a success. Don’t worry, you’re not alone! This is one of the biggest questions people ask when they start exploring fertility treatments. The good news? We’re going to break it all down for you in a way that’s easy to understand, packed with the latest info, and loaded with practical tips to help you feel more confident.
IVF can feel like a rollercoaster, but understanding the role of follicles is like getting a map to navigate the ride. Whether you’re just starting out or you’ve already got an appointment booked, this guide will give you a clear picture of what to expect, what the numbers mean, and how to boost your chances of seeing that positive pregnancy test. Let’s dive in!
What Are Follicles, Anyway?
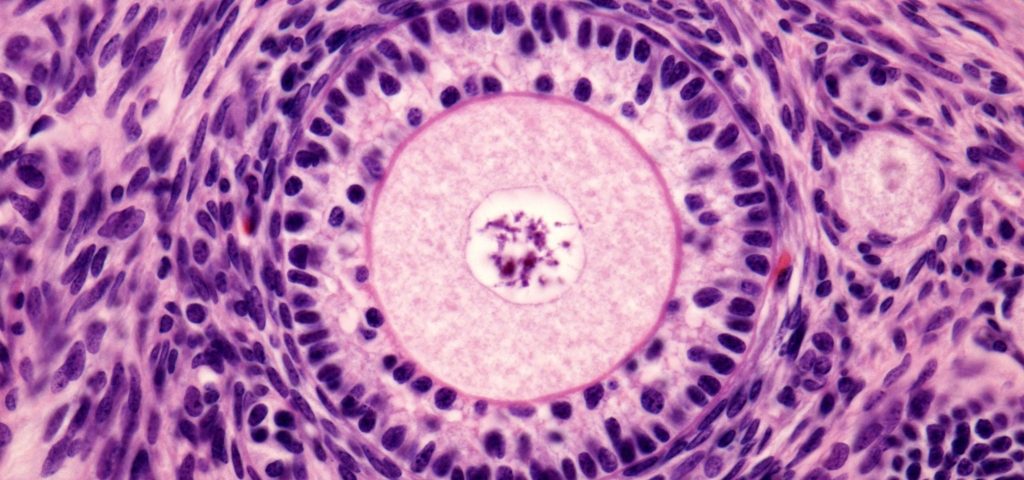
Picture your ovaries as little factories. Inside them, follicles are like tiny production units—small, fluid-filled sacs that each hold an immature egg. In a natural cycle, your body picks one follicle to grow and release an egg during ovulation. But with IVF, the goal is to get multiple follicles going at once, so you have more eggs to work with. More eggs mean more chances to create healthy embryos, which is the whole point of this process.
During IVF, doctors use medications to kick those factories into high gear. They’ll monitor how many follicles are growing and how big they get using ultrasound scans. The number and size of these follicles can tell a lot about how your body’s responding and what your odds of success might be. But here’s the catch: it’s not just about quantity—quality matters too. So, how many follicles should you aim for? Let’s explore that next.
The Magic Number: How Many Follicles Are Ideal for IVF?
When it comes to IVF, there’s no one-size-fits-all answer to how many follicles you need. Every person’s body is different, and what works for one might not work for another. That said, fertility experts have some general benchmarks based on years of research and real-world results.
The Sweet Spot: 4 to 15 Mature Follicles
Most clinics aim for 4 to 15 mature follicles before they trigger ovulation (that’s when they give you a shot to make the eggs ready for retrieval). Why this range? It’s a balance between getting enough eggs to increase your chances of success and avoiding risks like ovarian hyperstimulation syndrome (OHSS), which can happen if too many follicles develop.
- Fewer than 4 follicles: If you’ve got just 1 or 2, your doctor might suggest canceling the cycle or adjusting your meds for next time. It’s not impossible to succeed with fewer, but the odds of getting a viable embryo drop since you’re working with fewer eggs.
- 15 or more follicles: This sounds great, right? Not always. Too many follicles can lead to OHSS, a condition where your ovaries swell and leak fluid into your body. It’s uncomfortable at best and dangerous at worst. Plus, having tons of eggs doesn’t always mean they’re all high quality.
What Research Says
A 2023 study from the American Society for Reproductive Medicine found that women with 8 to 12 mature follicles had the highest live birth rates per cycle—around 35% for those under 35. When the number dipped below 4, success rates fell to under 20%. On the flip side, going over 20 follicles didn’t boost success much and increased OHSS risk by 15%. So, the data backs up that middle ground as a pretty solid target.
Real Talk: It’s Personal
Your “ideal” number depends on your age, ovarian reserve (how many eggs you’ve got left), and how your body reacts to the meds. A 28-year-old with a strong reserve might do great with 10 follicles, while a 40-year-old with fewer eggs might still succeed with just 3 or 4 if they’re top-notch quality. It’s less about hitting a specific number and more about finding what works for you.
Quick Tip: Ask your doctor what they’re aiming for based on your specific situation. They’ll have a game plan tailored to your body!
Follicles vs. Eggs: What’s the Difference?
Here’s where it gets a little tricky. Not every follicle has an egg, and not every egg is mature enough to use. Think of follicles as gift boxes—some might be empty, and some might have a prize inside. During egg retrieval, doctors use a needle to pull out the contents of each follicle, hoping to find a mature egg in most of them.
- On average, about 70-80% of mature follicles (those over 16-20mm) contain a usable egg.
- Of those eggs, around 60-70% are mature enough to fertilize, depending on your age and health.
So, if you’ve got 10 follicles, you might end up with 7 or 8 eggs, and maybe 5 or 6 that can actually turn into embryos. It’s a numbers game, but it’s not an exact science. That’s why doctors like to see a decent number of follicles—it gives them more shots at the goal.
Fun Fact: Ever wonder why they don’t just count eggs on the ultrasound? Eggs are microscopic—way too tiny to see! The follicle size is the best clue they’ve got.
Why Follicle Size Matters Just as Much as Number
Okay, so you’ve got a bunch of follicles growing—awesome! But size is a big deal too. Follicles need to hit a certain size before they’re likely to have a mature, ready-to-go egg inside.
The Goldilocks Zone: 16-22mm
- Too small (under 14mm): These follicles probably don’t have mature eggs yet. Triggering ovulation too early might mean fewer usable eggs.
- Just right (16-22mm): This is when most eggs are mature and ready for retrieval. A 2025 study from Imperial College Healthcare found that follicles between 13-18mm at trigger time gave the highest yield of mature eggs—up to 85% success per follicle.
- Too big (over 23mm): If follicles get too large, the egg inside might over-mature or not fertilize well. Timing is everything!
Doctors use ultrasound to track follicle growth every few days during stimulation. When most of your follicles hit that 16-22mm sweet spot, they’ll give you the trigger shot to ripen those eggs for retrieval.
Pro Tip: Don’t stress if some follicles are smaller or bigger—your doctor’s looking at the overall picture, not perfection in every single one.
What If You Don’t Get Enough Follicles?
Let’s say your ultrasound shows only 2 or 3 follicles growing. It’s natural to feel disappointed, but it’s not game over. Here’s what might happen and what you can do:
Possible Scenarios
- Cancel the Cycle: If the numbers are too low, your doctor might call it off to save you time, money, and emotional energy. They could tweak your meds and try again next time.
- Go For It Anyway: Sometimes, even 1 or 2 high-quality eggs can lead to success. A friend of mine had just 3 follicles at 38, went ahead with retrieval, and now has a healthy toddler!
- Switch Gears: Your doctor might suggest using donor eggs or embryos if your ovarian response stays low after a few tries.
Boosting Your Follicle Count
If you’re not hitting the numbers you want, there are ways to nudge things along:
- Adjust Meds: Higher doses of follicle-stimulating hormone (FSH) or a different protocol might wake up more follicles.
- Lifestyle Tweaks: Cut back on stress, eat a diet rich in antioxidants (think berries and nuts), and get enough sleep. A 2024 study linked better sleep to a 10% increase in follicle response.
- Supplements: CoQ10 and DHEA have shown promise in improving egg quality and quantity, especially for women over 35. Check with your doctor first, though!
Interactive Quiz: How’s Your Follicle Game?
- Are you under 35? (Yes = +1 point, No = 0)
- Do you sleep 7+ hours a night? (Yes = +1, No = 0)
- Are you eating a balanced diet? (Yes = +1, No = 0)
- 3 points: You’re setting yourself up for a strong response!
- 1-2 points: A few tweaks could help.
- 0 points: Time to chat with your doc about lifestyle boosts.
Too Many Follicles: Is That a Problem?
What if your ovaries go into overdrive and you’ve got 20, 30, or more follicles? It’s a double-edged sword. On one hand, more eggs sound like a win. On the other, it can backfire.
The Risk of OHSS
Ovarian hyperstimulation syndrome happens when your ovaries overreact to the meds. Symptoms range from bloating and nausea to serious stuff like breathing trouble or blood clots. It’s rare (less than 5% of cycles), but it’s more likely if you’ve got 20+ follicles or super-high estrogen levels.
- Mild OHSS: A little discomfort, manageable with rest and hydration.
- Severe OHSS: Needs medical attention—think hospital stays and IV fluids.
Managing the Overload
- Freeze All: If your follicle count’s sky-high, your doctor might retrieve the eggs but freeze the embryos instead of transferring them right away. This lets your ovaries calm down.
- Lower Doses: Next cycle, they might dial back the meds to keep things under control.
- Monitor Closely: Extra ultrasounds and blood tests can catch OHSS early.
Real-Life Example: Sarah, 32, had 25 follicles in her first cycle. Her doctor froze all her embryos to avoid OHSS, and she transferred one a few months later—now she’s expecting twins!
Age and Follicles: How They’re Connected
Your age plays a huge role in how many follicles you’ll get and how good those eggs are. Here’s the breakdown:
Under 35
- Follicle Count: Often 10-20 with stimulation.
- Success Rate: Around 45-50% live birth rate per cycle.
- Why: Younger ovaries have more eggs and better quality.
35-40
- Follicle Count: Drops to 5-15 on average.
- Success Rate: 30-35% per cycle.
- Why: Egg quantity and quality start declining.
Over 40
- Follicle Count: Might be 1-8, sometimes fewer.
- Success Rate: 10-15% with your own eggs.
- Why: Ovarian reserve shrinks, and egg quality takes a hit.
Data Point: The CDC’s 2024 IVF Success Estimator shows that women over 40 with 5+ follicles still have a 12% chance per cycle—low, but not zero. Using donor eggs bumps that up to 50%+, no matter your age.
Hopeful Note: Age isn’t everything. I’ve seen women in their early 40s with low counts beat the odds with just a couple of stellar eggs.
Antral Follicles: Your Starting Line
Before you even start IVF meds, your doctor might do a baseline ultrasound to count your antral follicles—the small, resting follicles visible at the start of your cycle. This gives a sneak peek at your ovarian reserve.
What’s a Good Antral Count?
- 15-30: You’re likely to respond well to stimulation.
- 8-14: Average response—still solid odds.
- Under 8: Might mean a lower response, but quality can still win out.
A 2023 study from Yale Medicine found that women with antral counts of 10+ had a 40% higher egg yield than those under 5. It’s not a perfect predictor, but it’s a helpful clue.
Action Step: Ask for your antral follicle count at your first consult. It’s a great convo starter with your doctor about what to expect.
Quality Over Quantity: The Unsung Hero
Here’s a truth bomb: 20 follicles don’t mean much if the eggs inside are duds. Egg quality—how healthy and genetically normal they are—is just as critical as the number you get.
What Makes an Egg “Good”?
- Chromosomes: Normal ones (23 pairs) are key for a healthy embryo.
- Energy: Eggs need strong mitochondria (their power plants) to develop.
- Age Factor: Younger eggs are more likely to check these boxes.
Boosting Quality
- Antioxidants: Foods like spinach, salmon, and dark chocolate fight oxidative stress, which can harm eggs.
- Stress Less: High cortisol can mess with egg development. Yoga or a good book might help more than you think.
- Timing: A 2025 study from Imperial College suggests triggering when more follicles are 13-18mm (not just the biggest ones) ups the mature egg count by 20%.
Interactive Checklist: Egg Quality Boosters
- ✔️ Eat a rainbow of fruits and veggies daily.
- ✔️ Get 30 minutes of light exercise most days.
- ❌ Skip the late-night caffeine binges.
- ❌ Don’t skimp on sleep—aim for 7-8 hours.
The IVF Follicle Journey: Step by Step
Wondering how follicles fit into the whole IVF process? Here’s a simple rundown:
- Stimulation (Days 1-10): You take meds like FSH to grow those follicles. Ultrasounds track their progress.
- Monitoring: Every few days, your doctor checks size and number—aiming for that 16-22mm range.
- Trigger Shot: When enough follicles are ready, you get a shot (usually hCG) to mature the eggs.
- Retrieval (36 Hours Later): Doctors collect the eggs from the follicles using a needle guided by ultrasound.
- Fertilization: Eggs meet sperm in the lab, and embryos start growing.
Timeline Tip: Stimulation usually lasts 8-14 days, but it’s flexible based on how your follicles respond.
Unique Angle: The Emotional Side of Follicle Counts
Most articles focus on the science, but let’s talk about the feelings. Seeing a low follicle count on that ultrasound screen can hit hard—like a punch to the gut. You might think, “Is this my fault?” or “Will this ever work?” On the flip side, a high count can spark hope, then anxiety if OHSS looms.
Coping Tips
- Talk It Out: A therapist or support group can lighten the load. I’ve heard amazing stories from IVF forums where people found strength in shared struggles.
- Celebrate Small Wins: Even 3 follicles is progress—focus on what’s working.
- Lean on Your Team: Your doctor’s there to guide you, not judge. Ask all the questions!
Poll: How Did Your Last Ultrasound Make You Feel?
- A) Hopeful and excited
- B) Nervous but optimistic
- C) Disappointed or stressed
(Share your answer in your head—or with a friend!)
Beyond the Numbers: Other Factors in IVF Success
Follicles are a big piece of the puzzle, but they’re not the whole picture. Here’s what else plays a role:
- Sperm Quality: Even the best eggs need a strong partner to make an embryo.
- Uterine Health: A cozy, receptive lining is key for implantation.
- Lab Skills: The embryologist’s expertise can make or break fertilization rates.
A 2024 report from the HFEA (UK’s fertility authority) showed that clinics with top-notch labs had 10% higher success rates, even with similar follicle counts. So, picking a solid clinic matters!
Fresh vs. Frozen: Does Follicle Count Change the Game?
Some folks do a fresh embryo transfer right after retrieval, while others freeze everything for later. Does follicle count affect this choice?
- Fresh Transfer: Works well with 8-15 follicles—enough eggs, low OHSS risk.
- Frozen Transfer: Often used with high counts (20+) to avoid OHSS, or if you’re banking embryos. Success rates are nearly identical to fresh these days, thanks to better freezing tech.
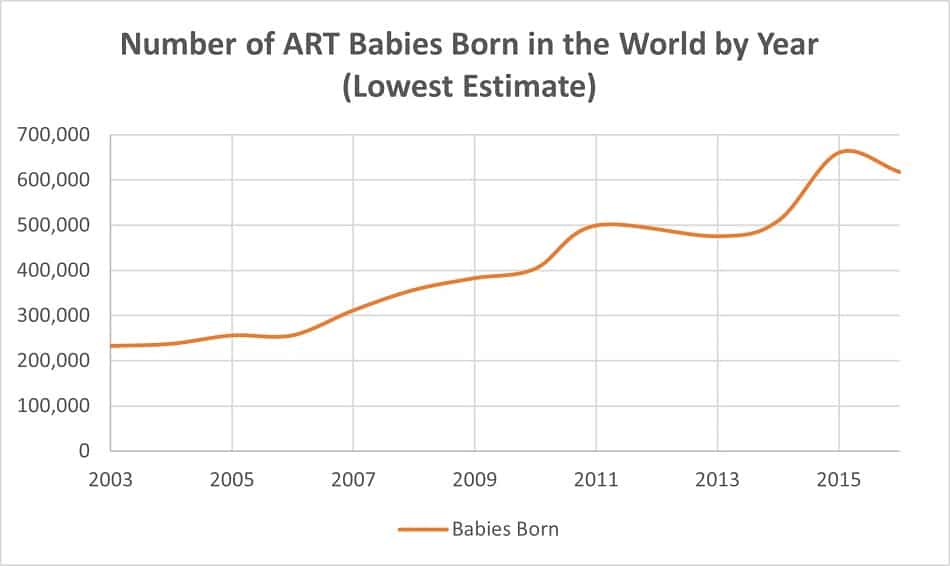
Data Nugget: A 2025 CDC report found frozen transfers from cycles with 10+ follicles had a 38% live birth rate—pretty close to fresh at 40%.
Mini Case Studies: Follicles in Action
Let’s peek at some real (but anonymized) stories to see how follicle counts play out:
- Jess, 29: 12 follicles, 9 eggs, 6 embryos. Fresh transfer worked—baby boy at 39 weeks!
- Maria, 37: 5 follicles, 3 eggs, 1 embryo. Frozen transfer after a second cycle—pregnant with twins.
- Lila, 42: 2 follicles, 1 egg, no embryos. Switched to donor eggs—success on the first try.
These show that follicle numbers set the stage, but the ending’s up to a mix of factors.
Latest Trends: What’s New in Follicle Science?
IVF’s always evolving, and 2025’s brought some cool updates:
- AI Timing: A study from Imperial College used AI to pinpoint the best trigger time based on follicle sizes (13-18mm), boosting mature egg yields by 20%.
- Natural Cycle IVF: For low responders, skipping heavy meds and working with 1-2 natural follicles is gaining traction—less stress, lower cost.
- Microbiome Link: Early research suggests a healthy gut might improve follicle response. Probiotics, anyone?
Prediction: In a few years, we might see personalized follicle targets based on DNA or gut health—wild, right?
Your Follicle Action Plan
Ready to take charge? Here’s how to make the most of your follicle game:
- Know Your Baseline: Get that antral count and talk goals with your doctor.
- Prep Your Body: Eat well, sleep deep, and chill out—your ovaries will thank you.
- Ask Questions: “What’s my target follicle number?” “How’s my egg quality looking?”
- Stay Flexible: High or low counts—there’s a plan for every scenario.
Final Thought: Follicles are just one part of your IVF story. Whether you get 3 or 30, it’s about working with what you’ve got and keeping hope alive. You’ve got this!