How Much Is IVF in Florida? Your Complete Guide to Costs, Options, and Insights
April 23, 2025
Can You Take Metformin While Undergoing IVF?
April 23, 2025How Many Embryos Are Used in IVF? Your Complete Guide to Understanding the Numbers
In vitro fertilization (IVF) is a life-changing journey for so many people dreaming of starting a family. If you’re exploring this option, you’ve probably wondered: How many embryos does it take to make IVF work? It’s a big question, and the answer isn’t one-size-fits-all. The number of embryos involved in IVF depends on a mix of science, personal circumstances, and even a little luck. Whether you’re just starting to research or you’re deep into the process, this guide will walk you through everything you need to know about embryos in IVF—how many are created, transferred, and what happens to the extras. Plus, we’ll dive into some fresh insights and practical tips you won’t find everywhere else.
Let’s break it down step by step, so you can feel confident and informed about what’s ahead.
What Happens to Embryos in IVF? The Basics You Need to Know
IVF is all about creating embryos outside the body and then giving them the best shot at becoming a pregnancy. But the process involves a lot more embryos than you might think. Here’s a quick rundown of how it works:
- Egg Retrieval: It starts with stimulating the ovaries to produce multiple eggs—usually 10-15, though this varies. These eggs are collected in a minor procedure.
- Fertilization: In the lab, those eggs meet sperm (either naturally or through a technique called ICSI, where a single sperm is injected into an egg). Not every egg turns into an embryo, but ideally, you’ll get several.
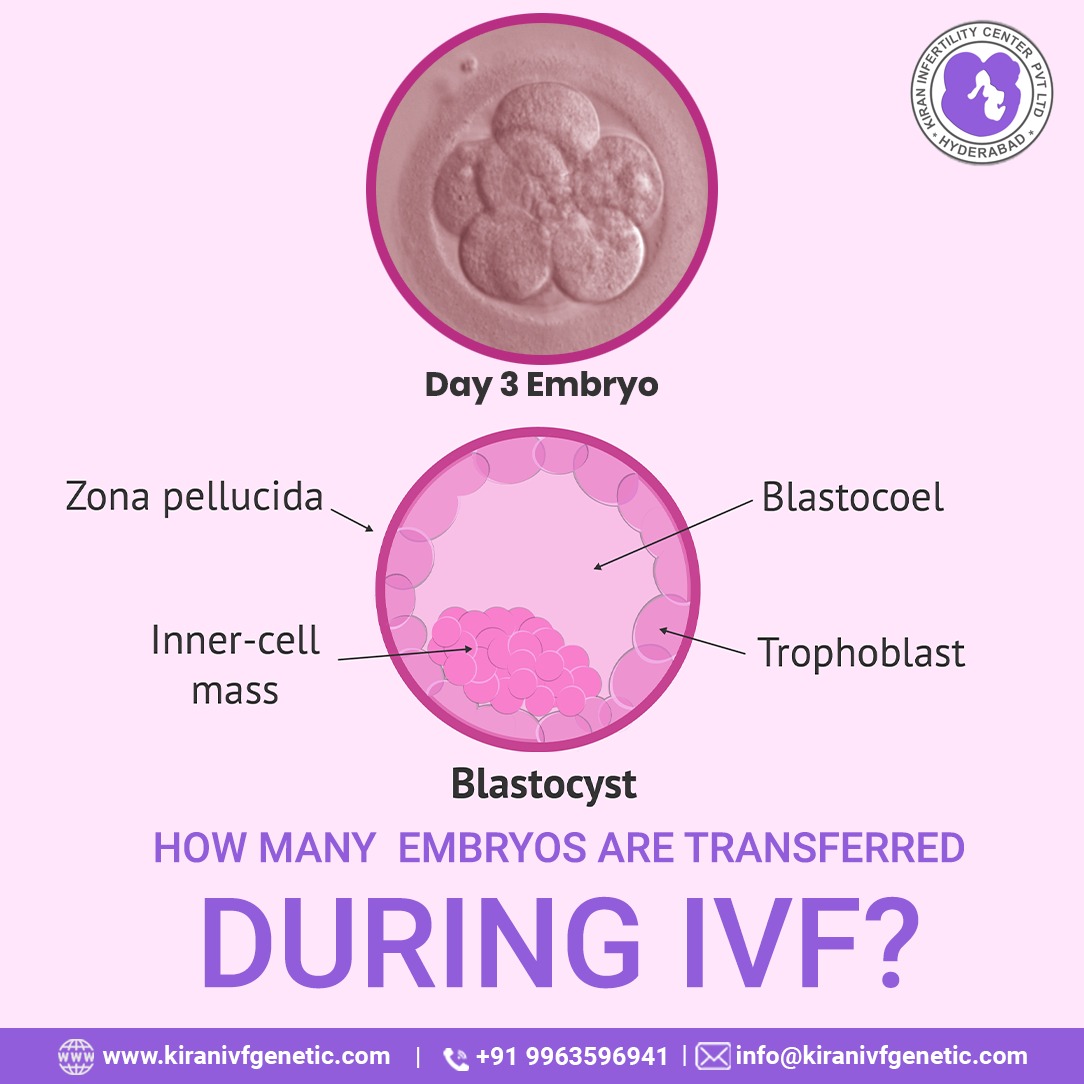
- Embryo Development: Over the next few days, the fertilized eggs grow into embryos. By day 5 or 6, they might reach the blastocyst stage—the point where they’re ready to implant in the uterus.
- Transfer: One or two embryos (sometimes more) are placed into the uterus, hoping they’ll stick and grow into a baby.
- Extras: Any leftover embryos can be frozen for later use, donated, or discarded, depending on your choice.
The number of embryos at each step isn’t set in stone. Some eggs don’t fertilize, some embryos stop growing, and not every transfer leads to pregnancy. That’s why IVF often involves working with multiple embryos to boost your chances.
How Many Embryos Are Typically Created in an IVF Cycle?
One of the first things people want to know is how many embryos they can expect from a single IVF cycle. The truth? It’s a numbers game, and it depends on a few key factors like age, egg quality, and sperm health.
On average, a woman under 35 might have 10-15 eggs retrieved in a cycle. About 70-80% of those eggs fertilize successfully, leaving you with 7-12 embryos. But here’s the catch: not all of them will make it to the blastocyst stage, which is when they’re strong enough for transfer or freezing. Studies show that only about 30-50% of fertilized eggs reach this point, so you might end up with 3-6 good-quality embryos.
For example:
- A 30-year-old with healthy eggs might get 12 eggs, 9 fertilize, and 4 become blastocysts.
- A 40-year-old might retrieve 8 eggs, with 5 fertilizing and only 2 reaching blastocyst stage.
Age plays a huge role here. According to the American Society for Reproductive Medicine (ASRM), younger women tend to produce more eggs and healthier embryos. After 35, egg quantity and quality drop, meaning fewer embryos overall. But don’t let that discourage you—modern IVF techniques are getting better at working with what you’ve got.
How Many Embryos Are Transferred During IVF?
Now, let’s talk about the big moment: the embryo transfer. How many embryos should you put back in? This is where things get personal—and a little tricky.
The Shift to Single Embryo Transfer (SET)
Back in the day, doctors often transferred two, three, or even more embryos to increase the odds of pregnancy. But that led to a lot of twins and triplets, which can be risky for both mom and babies. Today, the trend is moving toward single embryo transfer (SET), especially for younger women with healthy embryos.
The ASRM recommends:
- Women under 35: 1 embryo
- Women 35-37: 1-2 embryos
- Women 38-40: 2-3 embryos
- Women over 40: 3 or more, depending on embryo quality
Why the shift? SET cuts the chance of multiples (twins happen in less than 2% of SET cases, compared to 20-30% with two embryos). Plus, with tools like preimplantation genetic testing (PGT), doctors can pick the strongest embryo, making one enough.
Real-Life Example
Take Sarah, a 32-year-old who did IVF last year. Her doctor transferred one embryo after PGT showed it was chromosomally normal. She’s now 6 months pregnant with a single, healthy baby. Compare that to Lisa, 39, who transferred two embryos because her egg quality was lower. She got pregnant with twins—a joy, but also a higher-risk pregnancy.
What’s Right for You?
Your doctor will look at your age, embryo quality, and past IVF attempts. Want just one baby? SET might be your best bet. Hoping for twins? Transferring two could be an option, but talk it over carefully—multiple pregnancies come with challenges like preterm birth and extra medical costs.
What Happens to Extra Embryos? Options You Might Not Have Considered
If you’re lucky, you’ll end up with more embryos than you need for one transfer. So, what happens to the rest? This is a big decision, and it’s worth thinking about early on.
Freezing for the Future
Most people freeze their extra embryos—a process called cryopreservation. Frozen embryos have a great success rate, with pregnancy rates nearly matching fresh transfers (around 25-30% per cycle, per ASRM data). You can use them later for another baby or if the first try doesn’t work.
- Pros: Saves time and money (no need for another full IVF cycle).
- Cons: Storage fees (about $300-$500 a year) add up.
Donation: A Gift to Others or Science
You could donate your embryos to another couple struggling with infertility or to research. Embryo donation is less common but growing—over 1,000 babies are born this way each year in the U.S. Donating to science helps researchers improve IVF and study early human development.
- Pros: Feels meaningful; helps others.
- Cons: Emotional weight of giving up potential children.
Discarding Embryos
Some choose to discard unused embryos. This might happen if you’re done building your family or if the embryos aren’t viable. Clinics handle this respectfully, but it can feel heavy for some.
A Fresh Idea: Compassionate Transfer
Here’s something not everyone talks about: compassionate transfer. This is when leftover embryos are placed in the uterus at a time in your cycle when pregnancy is unlikely (like during your period). It’s a middle ground between keeping them frozen forever and discarding them outright. It’s rare, but some find it a comforting option.
Why Don’t All Embryos Make It? The Science Behind the Numbers
You might start with 10 embryos, but only a few—or none—lead to a baby. Why? It’s all about biology and a bit of chance.
Embryo Quality Matters
Not every embryo is a winner. Some have chromosomal issues (like extra or missing pieces of DNA) that stop them from growing. PGT can screen for this, but even then, only about 50-60% of embryos test normal, especially as you get older.
Implantation Challenges
Even a perfect embryo might not implant. The uterus has to be just right—think of it like planting a seed in soil that’s not quite ready. Hormones, lining thickness, and timing all play a part. Studies estimate that 70-85% of natural embryos don’t implant, and IVF isn’t much different.
The Drop-Off Rate
Here’s a simple breakdown of what might happen in one cycle:
- 12 eggs retrieved
- 9 fertilize
- 5 reach blastocyst
- 1-2 are transferred
- 0-1 implant successfully
That’s why doctors aim for multiple embryos—it’s a buffer against these natural losses.
Interactive Quiz: How Many Embryos Do You Think You’d Need?
Let’s make this fun! Take a quick quiz to guess how many embryos might be in your IVF future. Answer these questions, then check the results below:
- How old are you?
- A) Under 35
- B) 35-37
- C) 38-40
- D) Over 40
- How many kids do you want?
- A) Just 1
- B) 2 or more
- Are you okay with twins?
- A) Yes, bring it on!
- B) No, one at a time, please
Results:
- Mostly A’s: You might aim for 3-5 embryos, with a focus on SET for one healthy baby.
- Mix of A and B: You could end up with 5-8 embryos, planning for a couple kids over time.
- Mostly C’s or D’s: You might need 6-10 embryos to account for lower egg quality and multiple tries.
This is just a rough guess—your doctor will give you a personalized plan!
How Many Embryos Should You Aim For? A Practical Checklist
So, how do you decide how many embryos to shoot for? It’s about balancing your goals with reality. Here’s a checklist to help you figure it out:
✔️ Know Your Age: Younger? You might need fewer embryos. Over 38? Plan for more.
✔️ Set a Family Goal: One kid? Two? More embryos mean more options later.
✔️ Check Your Finances: Each cycle costs $12,000-$25,000. Freezing extras can save you from starting over.
✔️ Talk Risk: Multiples sound fun but can mean bed rest or NICU time. Are you ready?
✔️ Ask About PGT: Testing embryos upfront can cut the number you need by picking the best ones.
For instance, if you’re 34 and want two kids, you might aim for 6-8 embryos—enough for a couple tries now and a frozen stash for later.
Fresh Research: What’s New in Embryo Numbers for 2025?
IVF is always evolving, and 2025 brings some exciting updates that could change how many embryos you need.
AI Picks the Winners
Artificial intelligence is stepping up. New studies from 2024 show AI can predict which embryos are most likely to implant with up to 85% accuracy—better than human embryologists in some cases. This means you might need fewer embryos overall, as the tech zeroes in on the strongest ones.
Better Freezing Tech
Vitrification (a super-fast freezing method) is getting even more precise. A 2023 study found that frozen embryos now have a 5-10% higher survival rate than five years ago. That’s good news if you’re banking extras for the future.
Mini-IVF: Fewer Eggs, Smarter Choices
Mini-IVF uses lower doses of drugs to get 3-5 eggs instead of 10-15. It’s gentler and cheaper, and early 2025 data suggests it’s just as effective for some women, especially those sensitive to hormones. Fewer eggs might mean fewer embryos, but the focus is on quality over quantity.
Unique Insight: The Emotional Side of Embryo Numbers
Here’s something you won’t find in every article: the emotional rollercoaster of counting embryos. Every number—eggs retrieved, embryos created, ones that make it—feels like a tiny victory or a gut punch. When I talked to my friend Jen, who did IVF in 2023, she said, “I started with 14 eggs and ended with 3 embryos. Each drop felt like losing a piece of hope.”
It’s not just science—it’s personal. Give yourself grace to feel it all, and lean on support groups or a counselor if the numbers start to weigh you down.
Poll: What Would You Do With Extra Embryos?
Let’s hear from you! If you had leftover embryos, what would you choose? Vote below and see what others think:
- A) Freeze them for later
- B) Donate them to another couple
- C) Give them to science
- D) Discard them
- E) Try a compassionate transfer
Check back next week for the results—your input could spark a great discussion!

How to Boost Your Embryo Count: Tips You Can Use
Want to maximize your embryo numbers? While some things (like age) are out of your control, others aren’t. Here are some practical steps backed by science:
- Eat Smart: A Mediterranean diet—think fish, nuts, and veggies—can improve egg quality. A 2022 study linked it to 20% more viable embryos.
- Cut Stress: High cortisol levels mess with hormones. Yoga or meditation might give you an edge—research shows relaxed women have better IVF outcomes.
- Supplement Wisely: Coenzyme Q10 (CoQ10) is trending. A 2024 trial found it boosted embryo quality in women over 35 by 15%.
- Sleep Well: Aim for 7-8 hours. Poor sleep disrupts ovulation, which can mean fewer eggs and embryos.
Talk to your doctor before changing anything, but these tweaks could tip the scales.
Case Study: A Couple’s Journey With Embryo Numbers
Meet Alex and Maria, a couple in their late 30s. They did IVF in 2024 and shared their story with me. Maria retrieved 10 eggs, 7 fertilized, and 3 made it to blastocyst. They transferred one—negative. The second try with a frozen embryo worked, and they’re expecting a girl. The third embryo? Still frozen, waiting for baby #2.
Their takeaway? “We wished we’d pushed for more eggs upfront,” Alex said. “Three embryos felt tight.” Their experience shows why planning for extras can ease the pressure.
The Big Picture: How Many Embryos Equal Success?
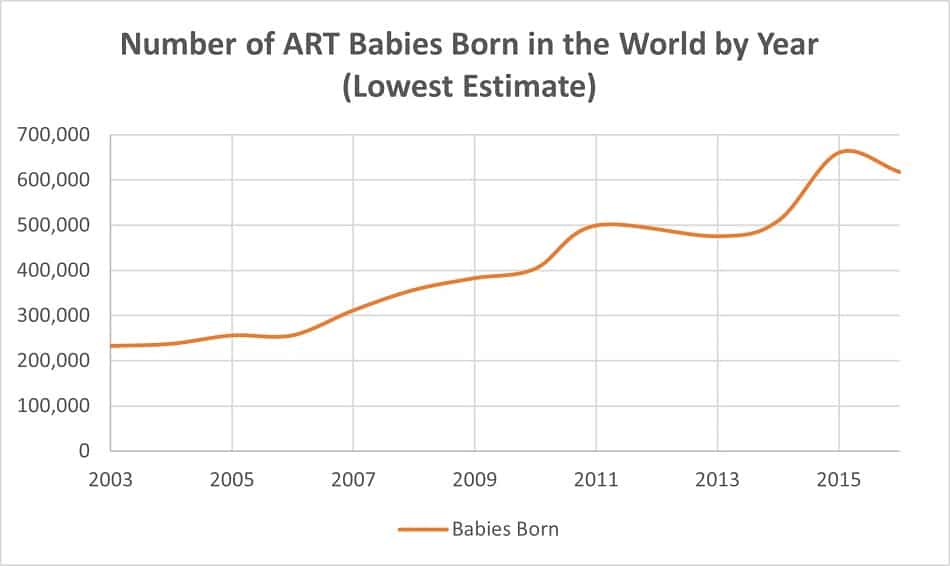
There’s no magic number that guarantees a baby. Some get pregnant with one embryo; others need multiple cycles. Data from the CDC (2023) says the average live birth rate per embryo transferred is 25-30% for women under 35, dropping to 10-15% over 40. But here’s the kicker: 70% of IVF patients need more than one cycle to succeed.
So, how many embryos do you need? Enough to keep going until it works—whether that’s 2, 5, or 10. It’s less about the total and more about having options.
Wrapping It Up: Your Embryo Journey Starts Here
IVF is a marathon, not a sprint, and the number of embryos you work with shapes the whole experience. From how many you create to what you do with the extras, every step is a chance to take control of your path to parenthood. Armed with the latest research, practical tips, and a little emotional prep, you’re ready to tackle this with confidence.
Got questions? Drop them in the comments—I’d love to chat more about your IVF adventure!