Can a Woman Self-Administer Fertility Drugs for IVF?
April 19, 2025
Does Blue Cross Blue Shield Cover IVF?
April 19, 2025Does Aetna Cover IVF? Your Guide to Understanding Fertility Benefits
Navigating the world of health insurance can feel like trying to solve a puzzle with missing pieces—especially when it comes to something as personal and complex as fertility treatments. If you’re wondering whether Aetna covers in vitro fertilization (IVF), you’re not alone. Millions of people across the U.S. face infertility challenges, and figuring out what your insurance will pay for is a big part of the journey. Let’s dive into this topic with a fresh perspective, breaking it down step-by-step so you can feel confident about what to expect.
IVF is a life-changing option for many, but it’s also expensive and emotionally taxing. The good news? Aetna, one of the nation’s largest insurers, does offer coverage for IVF in many cases—but the details depend on your specific plan, where you live, and a few other factors. This article will walk you through everything you need to know, from the basics of Aetna’s policies to practical tips for maximizing your benefits. Plus, we’ll explore some angles that don’t always get enough attention, like how recent policy changes affect coverage and what to do if your claim gets denied.
What Is IVF, and Why Does Insurance Matter?
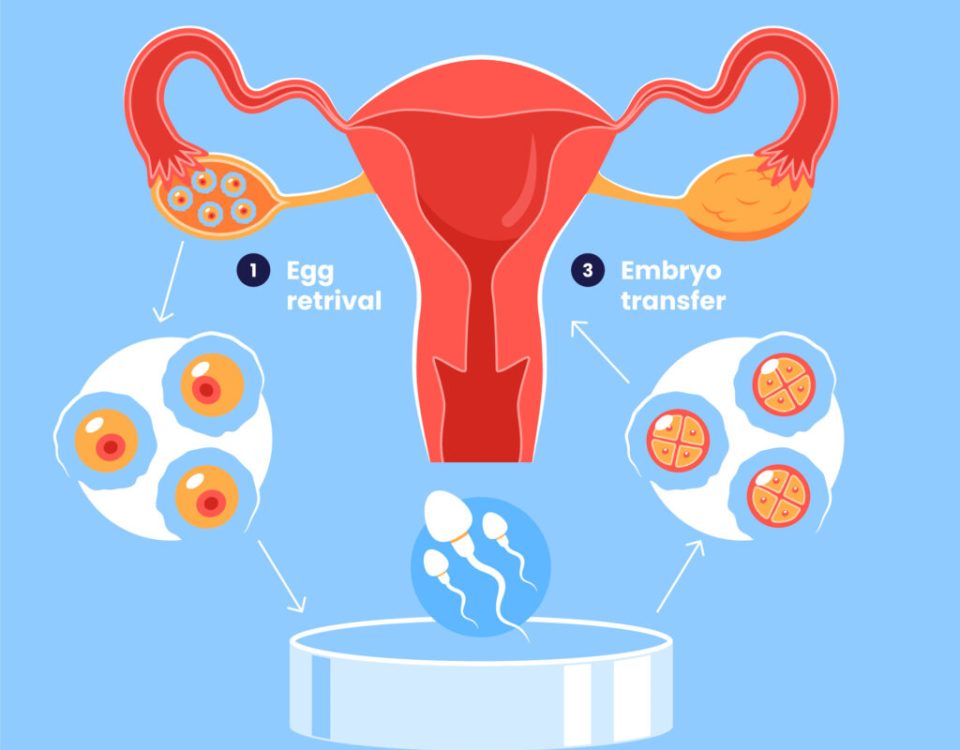
IVF, or in vitro fertilization, is a process where eggs are retrieved from the ovaries, fertilized with sperm in a lab, and then transferred into the uterus. It’s often a go-to solution for couples struggling with infertility due to blocked fallopian tubes, low sperm count, or unexplained issues. A single cycle can cost anywhere from $12,000 to $20,000, not including medications, which can add another $3,000 to $5,000. For many, that’s a huge financial hurdle—making insurance coverage a game-changer.
Insurance matters because it can turn an out-of-reach dream into a realistic possibility. Without it, you might be stuck saving for years or taking out loans. Aetna serves around 36 million people, so if you’re one of them, understanding their IVF coverage could save you thousands and a lot of stress. But here’s the catch: not all plans are created equal, and Aetna’s policies have evolved over time to reflect new laws, societal shifts, and member needs.
Does Aetna Cover IVF? The Short Answer
Yes, Aetna often covers IVF—but it’s not a simple yes or no. Coverage depends on your specific health plan, whether it’s through an employer, an individual policy, or a government program like Medicaid. Some plans include IVF as part of a broader infertility benefit, while others might limit it or exclude it entirely. To get the full picture, you’ll need to check your plan documents or call Aetna’s Member Services (the number’s on your insurance card).
Here’s what Aetna typically offers for IVF:
- Diagnostic Testing: Blood tests, ultrasounds, and semen analysis to figure out why conception isn’t happening.
- Basic Treatments: Things like intrauterine insemination (IUI) or fertility drugs might be covered before IVF is considered.
- IVF Cycles: If your plan includes advanced reproductive technology (ART), IVF may be covered, sometimes with a limit on the number of cycles (e.g., 3 attempts) or a lifetime maximum (e.g., $25,000).
But there’s more to it than that. Let’s break it down further.
How Aetna Decides IVF Coverage
Aetna doesn’t just hand out IVF benefits to everyone. They use specific criteria to determine if you qualify, and these rules can vary by plan. Here’s what they usually look at:
Your Plan Type
- Employer-Sponsored Plans: If you get Aetna through work, your employer decides what’s covered. Some companies opt for generous fertility benefits to attract employees, while others stick to the basics. For example, a tech firm might offer unlimited IVF cycles, but a small business might not cover it at all.
- Individual Plans: If you bought your plan directly, coverage depends on what you signed up for and your state’s laws.
- Federal or Medicaid Plans: These follow strict government guidelines, and IVF is rarely included unless mandated by state law.
Medical Necessity
Aetna often requires proof that IVF is medically necessary. This might mean:
- You’ve tried conceiving naturally for 12 months (or 6 months if you’re over 35) without success.
- You’ve already attempted less invasive treatments, like IUI or fertility drugs, and they didn’t work.
- There’s a diagnosed condition (e.g., endometriosis or low ovarian reserve) that makes IVF the best option.
Precertification
Before you start IVF, your doctor usually needs to get approval from Aetna. This step, called precertification, involves submitting medical records to show why IVF is needed. Without it, you could end up paying out of pocket.
State Laws
Where you live plays a big role. As of 2025, 21 states have laws requiring some level of infertility coverage, and 15 of them specifically mandate IVF benefits. For example:
- New York: Requires large group plans to cover up to 3 IVF cycles.
- California: Doesn’t mandate IVF coverage but requires insurers to offer it as an option.
- Texas: No mandate, so it’s up to your plan.
If you’re in a mandate state, Aetna has to follow those rules for certain plans. Check your state’s insurance department website for details.
What Aetna’s IVF Coverage Might Look Like
Let’s say your plan does cover IVF. What can you expect? Here’s a breakdown based on Aetna’s general policies and recent updates:
Covered Services
- Egg Retrieval and Fertilization: The core IVF process is often included.
- Embryo Transfer: Placing the embryo in the uterus is typically covered.
- Medications: Fertility drugs like Clomid or injectables might be partially covered, though you’ll likely pay a copay or coinsurance.
- Preimplantation Genetic Testing (PGT): If you have a genetic condition, this might be covered under some plans.
Limits and Caps
- Cycle Limits: Some plans cap IVF at 2 or 3 cycles. A “cycle” usually means one full round of egg retrieval and transfer.
- Lifetime Maximum: You might see a dollar limit, like $20,000 or $30,000, for all infertility treatments combined.
- Age Restrictions: Coverage might stop at age 40 or 45, depending on the plan.
Out-of-Pocket Costs
Even with coverage, you’re not off the hook entirely. Expect to pay:
- Deductibles: The amount you pay before insurance kicks in (e.g., $1,000-$5,000).
- Coinsurance: A percentage of the cost (e.g., 20% of a $15,000 cycle = $3,000).
- Non-Covered Services: Things like donor eggs or surrogacy are often excluded.
Real-Life Example
Sarah, a 34-year-old teacher in New Jersey, has Aetna through her school district. Her plan covers 3 IVF cycles with a $25,000 lifetime max. After meeting her $2,000 deductible, Aetna paid 80% of her $18,000 cycle, leaving her with $3,600 out of pocket. Her meds cost $4,000, but her prescription plan covered half. Total cost to her: $5,600—still a lot, but way less than the full price.
Recent Changes to Aetna’s Fertility Coverage
Aetna’s been making waves with its fertility policies lately, and that’s good news for many. Here are two big updates from 2024-2025 that could affect IVF coverage:
Expanded IUI Access
In September 2024, Aetna became the first major insurer to cover intrauterine insemination (IUI) as a standard medical benefit for all eligible plans, regardless of sexual orientation or partner status. Why does this matter for IVF? IUI is often a stepping stone—cheaper and less invasive than IVF. If it works, you might not need IVF at all. If it doesn’t, it can help meet Aetna’s “medical necessity” requirements for IVF approval.
Settlement for LGBTQ+ Equity
In May 2024, Aetna settled a lawsuit claiming its old policies discriminated against LGBTQ+ members. Before, same-sex couples or single individuals had to pay for 6-12 IUI cycles out of pocket to prove infertility, while heterosexual couples just needed to try naturally. Now, Aetna’s updated its rules to ensure equal access to IVF and other treatments, no matter who you are. They also set aside $2 million to reimburse affected New York members.
These changes show Aetna’s responding to pressure from members, advocates, and legal challenges. It’s a sign they’re adapting to modern family-building needs—something other insurers might follow.
Interactive Quiz: Does Your Aetna Plan Cover IVF?
Not sure where you stand? Take this quick quiz to get a sense of your coverage odds. Answer yes or no, and tally your points (1 for yes, 0 for no):
- Do you have an employer-sponsored Aetna plan with infertility benefits?
- Have you been trying to conceive for at least 6-12 months (depending on age)?
- Does your state mandate IVF coverage?
- Has your doctor recommended IVF as medically necessary?
- Are you under any age limits set by your plan (e.g., 45)?
Results:
- 4-5 points: Great chance of coverage—check your plan details!
- 2-3 points: Maybe—dig into your policy or call Aetna.
- 0-1 point: Less likely, but you might still have options (see below).
This isn’t official, but it’s a starting point to guide your next steps.
What If Aetna Doesn’t Cover IVF?
If your plan doesn’t include IVF, don’t lose hope. There are ways to work around it or push for coverage. Here’s what you can do:
Appeal a Denial
If Aetna rejects your IVF claim, you can appeal. Here’s how:
- Review the Denial Letter: It’ll explain why they said no (e.g., “not medically necessary”).
- Gather Evidence: Get a letter from your doctor explaining why IVF is your best shot, plus any test results.
- Submit the Appeal: File it online via Aetna’s member portal or mail it in (details are in your denial letter).
- Request a Review: If the appeal fails, ask for an independent third-party review—some states require this.
A 2023 study by the American Society for Reproductive Medicine found that 1 in 4 insurance appeals for fertility treatments succeeds when backed by strong medical evidence. Persistence pays off!
Explore Other Benefits
Even without IVF coverage, your plan might cover:
- Diagnostic Tests: To pinpoint the issue.
- Fertility Drugs: To boost ovulation or sperm production.
- IUI: Now standard for many Aetna plans, it’s a cheaper first step.
Look Beyond Aetna
- Employer Negotiation: Ask HR to add IVF benefits—big companies are increasingly open to this.
- State Programs: Some states (e.g., Maryland) offer grants for IVF.
- Financing: Clinics often have payment plans or discounts for self-pay patients.
Three Under-the-Radar Factors Affecting Aetna IVF Coverage
Most articles stick to the basics, but these lesser-known points can make a big difference:
1. Self-Funded vs. Fully Insured Plans
If your employer “self-funds” your Aetna plan (common with big companies), they—not Aetna—decide what’s covered. Fully insured plans follow Aetna’s standard policies and state laws. How to tell? Ask HR: “Is our plan self-funded?” If yes, your IVF coverage hinges on your employer’s choices, not just Aetna’s rules.
2. Fertility Preservation Coverage
Planning chemo or another treatment that could harm your fertility? Aetna often covers IVF for “iatrogenic infertility” (caused by medical procedures). This includes egg or sperm freezing before treatment starts. It’s a niche benefit, but it’s a lifeline for cancer patients or others facing similar challenges.
3. Network Restrictions
Aetna might require you to use specific providers, like their “Institutes of Excellence” for infertility. Going out-of-network could mean higher costs or no coverage. Call Aetna’s National Infertility Unit (1-800-575-5999) to find in-network clinics near you—they’ll also explain your benefits.
Practical Tips to Maximize Your Aetna IVF Benefits
Ready to take action? Here’s a step-by-step guide to get the most out of your coverage:
Step 1: Know Your Plan
- Log into Aetna.com and download your Summary Plan Description (SPD).
- Look for sections on “infertility,” “ART,” or “reproductive services.”
- Note any limits, exclusions, or precertification rules.
Step 2: Talk to Your Doctor
- Ask for a clear diagnosis and treatment plan.
- Have them submit precertification to Aetna—most clinics handle this for you.
Step 3: Call Aetna
- Dial Member Services and ask:
- “Does my plan cover IVF?”
- “What are the requirements and limits?”
- “Are there in-network fertility specialists I should use?”
Step 4: Budget Smartly
- Estimate your out-of-pocket costs (deductible + coinsurance).
- Set up a Health Savings Account (HSA) if you have a high-deductible plan—IVF expenses qualify.
Step 5: Stay Updated
- Policies change. Aetna’s 2024 IUI expansion and LGBTQ+ settlement prove it. Check back yearly or when your plan renews.
✔️ Pro Tip: Record your calls with Aetna (with permission) to keep track of what’s promised.
❌ Don’t: Assume coverage without confirming—verbal promises don’t override your plan documents.
Poll: What’s Your Biggest IVF Concern?
We’d love to hear from you! Pick one:
- A) Cost of treatment
- B) Insurance coverage confusion
- C) Emotional stress
- D) Finding the right doctor
Drop your answer in the comments below—it’ll help us tailor future articles to your needs!
The Bigger Picture: IVF Coverage Trends in 2025
Aetna’s not operating in a vacuum. Fertility coverage is a hot topic right now, driven by:
- Workplace Benefits: A 2024 Mercer survey found 45% of employers with 500+ workers offer IVF coverage, up from 36% in 2021. Companies see it as a perk to keep talent.
- Legal Shifts: Post-2022 Dobbs decision, reproductive rights (including IVF) are under scrutiny. Some states are pushing to protect or expand access.
- Social Media Buzz: Platforms like X show growing chatter about IVF affordability, with users praising Aetna’s IUI move but calling for more transparency on costs.
What does this mean for you? Pressure’s building on insurers like Aetna to broaden fertility benefits. If your plan’s lacking now, it might improve in the next renewal cycle.
Unique Insight: My Mini-Analysis of Aetna IVF Costs
I crunched some numbers based on public Aetna data and clinic pricing to give you a fresh angle. For a typical $15,000 IVF cycle:
- With Coverage (80% after $2,000 deductible): You pay $5,000.
- Without Coverage: Full $15,000.
- Savings: $10,000 per cycle.
Now, assume 1 in 3 cycles succeeds (a rough average from CDC data). With 3 covered cycles, your total out-of-pocket could be $15,000 for a baby—versus $45,000 without insurance. That’s a 67% cost reduction. Not every article does the math, but it shows why fighting for coverage is worth it.
Emotional Side of IVF and Insurance
Let’s get real: IVF isn’t just about money. It’s a rollercoaster of hope, disappointment, and resilience. Dealing with insurance adds another layer of stress—waiting for approvals, decoding denials, or realizing your dream’s out of reach. A 2023 study in Fertility and Sterility found that 60% of IVF patients reported insurance issues as a major source of anxiety.
Here’s a tip from someone who’s been there: Build a support system. Whether it’s a friend, a therapist, or an online group, having people to lean on makes the process less lonely. And if Aetna’s giving you a headache, vent to them—they might not fix it, but it’ll feel good.
Wrapping Up: Your Next Move
So, does Aetna cover IVF? For many, yes—but it’s a puzzle you’ll need to piece together with your plan details, doctor’s input, and a little persistence. Start by checking your coverage, talking to Aetna, and exploring every option if IVF’s not included. The landscape’s shifting, and with moves like Aetna’s 2024 updates, access is slowly getting better.
You’ve got this. Whether it’s your first call to Member Services or your third appeal letter, every step brings you closer to your goal. And if you’ve got a story to share—maybe how Aetna helped (or didn’t)—drop it in the comments. It could inspire someone else on this journey.