How Is IVF Done? Your Complete Guide to In Vitro Fertilization
April 17, 2025
Does IVF Hurt? A Deep Dive into the Physical and Emotional Journey
April 17, 2025How Does IVF Work? Your Complete Guide to In Vitro Fertilization
In vitro fertilization, or IVF, is like a superhero for people dreaming of starting a family but facing roadblocks. It’s a process that’s helped millions of hopeful parents bring babies into the world, and it’s way more common than you might think—about 2.5% of babies born in the U.S. today come from IVF. But how does it actually work? If you’re curious about the steps, the science, or what it feels like to go through it, you’re in the right place. This guide will walk you through everything, from the basics to the nitty-gritty details, with some fresh insights you won’t find everywhere else.
IVF isn’t just a medical procedure—it’s a journey. Whether you’re dealing with infertility, planning for the future, or helping a friend understand their options, knowing how it all comes together can make it less mysterious. Let’s dive in and explore how this incredible process turns hope into tiny humans.
What Is IVF, Anyway?
IVF stands for “in vitro fertilization,” which is a fancy way of saying “fertilization in a glass.” The “glass” part refers to a lab dish where eggs and sperm meet, not inside a person’s body like in natural conception. It’s part of a bigger group of tools called assisted reproductive technology (ART), designed to help people who can’t get pregnant on their own.
Picture this: normally, an egg and sperm team up in a fallopian tube after ovulation, then travel to the uterus to grow into a baby. But sometimes, that teamwork doesn’t happen—maybe the tubes are blocked, the sperm can’t swim well, or the eggs need a little extra help. That’s where IVF steps in, taking the process outside the body and giving it a boost.
Since the first IVF baby, Louise Brown, was born in 1978, the technology has come a long way. Today, over 8 million babies worldwide owe their start to IVF. It’s not just for couples with infertility anymore—single parents, same-sex couples, and people using surrogates rely on it too.
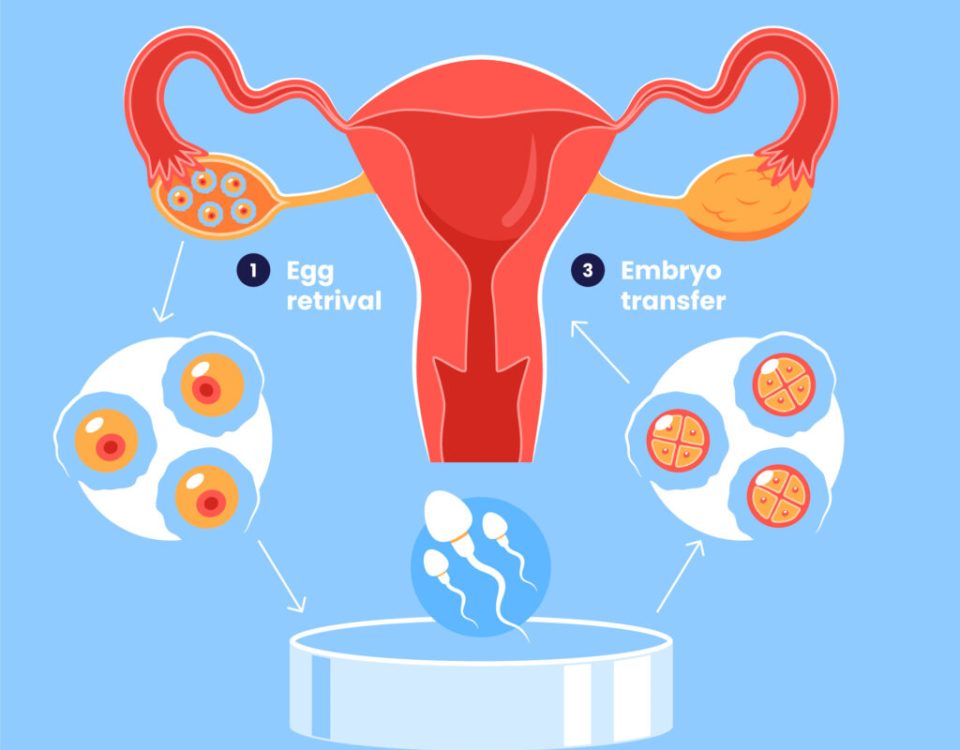
The Big Picture: How IVF Works Step by Step
IVF isn’t a one-and-done deal—it’s a series of steps that can take about 4 to 6 weeks per cycle. Each part builds on the last, like a recipe for your favorite dish. Here’s the rundown of how it all happens:
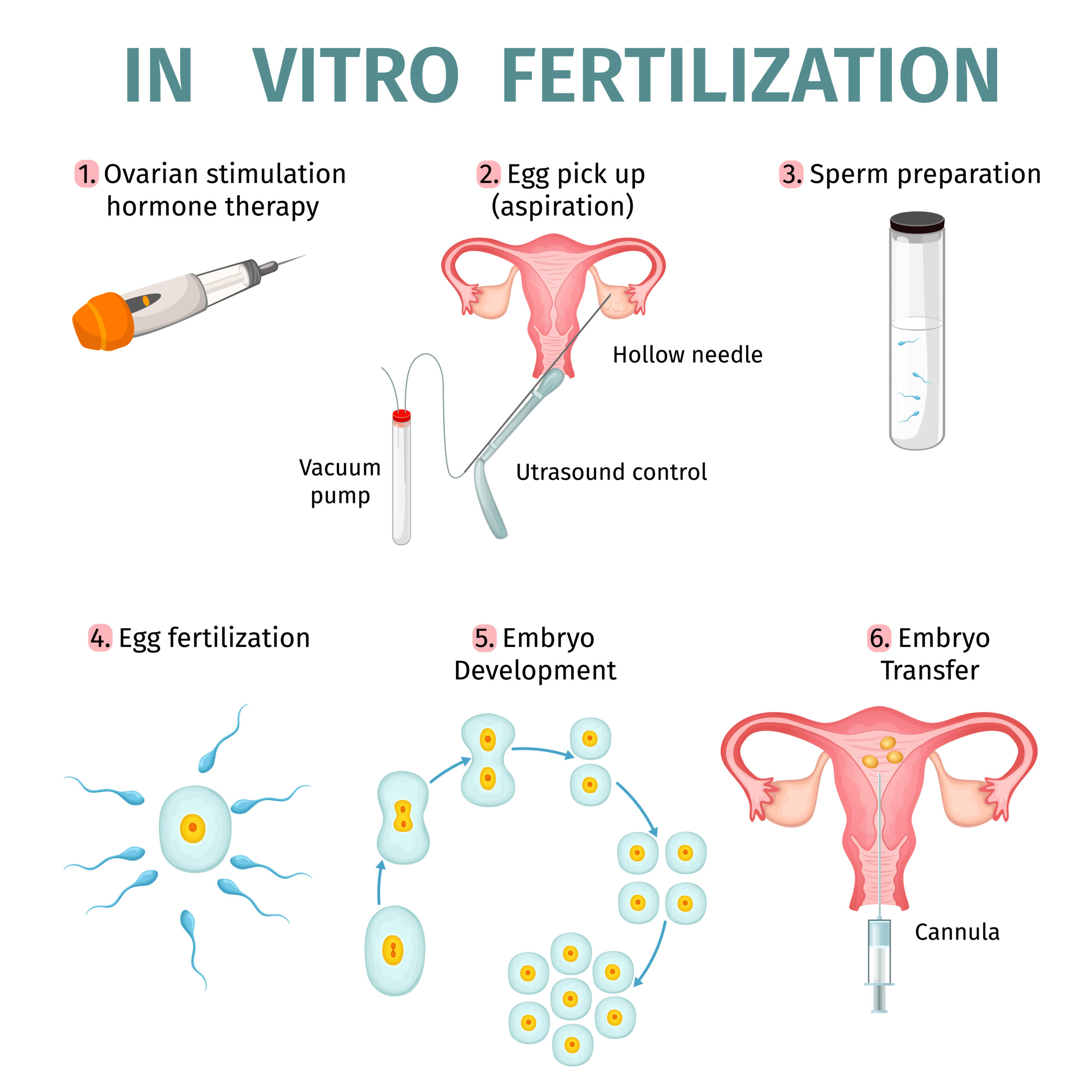
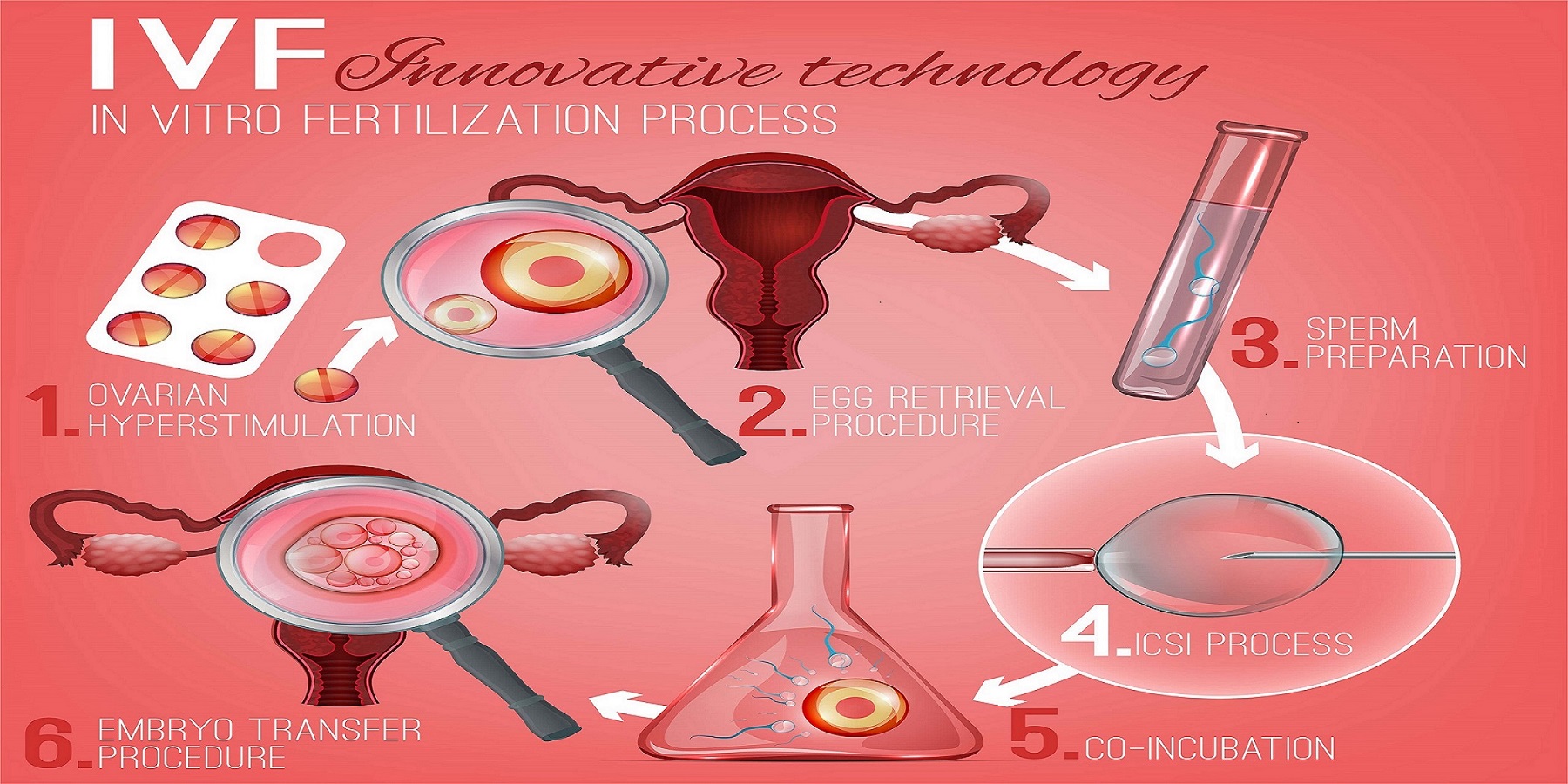
Step 1: Boosting Egg Production
The first step is getting your ovaries to make more eggs than usual. Normally, your body releases one egg a month during ovulation. With IVF, doctors use fertility drugs—think of them as cheerleaders for your ovaries—to encourage several eggs to grow at once. More eggs mean more chances for success.
You’ll take these meds (usually shots you give yourself at home) for about 8 to 14 days. During this time, your doctor keeps an eye on things with ultrasounds and blood tests to check hormone levels and see how many egg sacs (follicles) are growing. It’s a bit like watching a garden bloom—you want as many healthy flowers as possible.
✔️ Tip: Keep a small cooler handy for storing your meds—some need to stay cold!
❌ Don’t: Skip doses, even if the shots sting a little. Consistency is key.
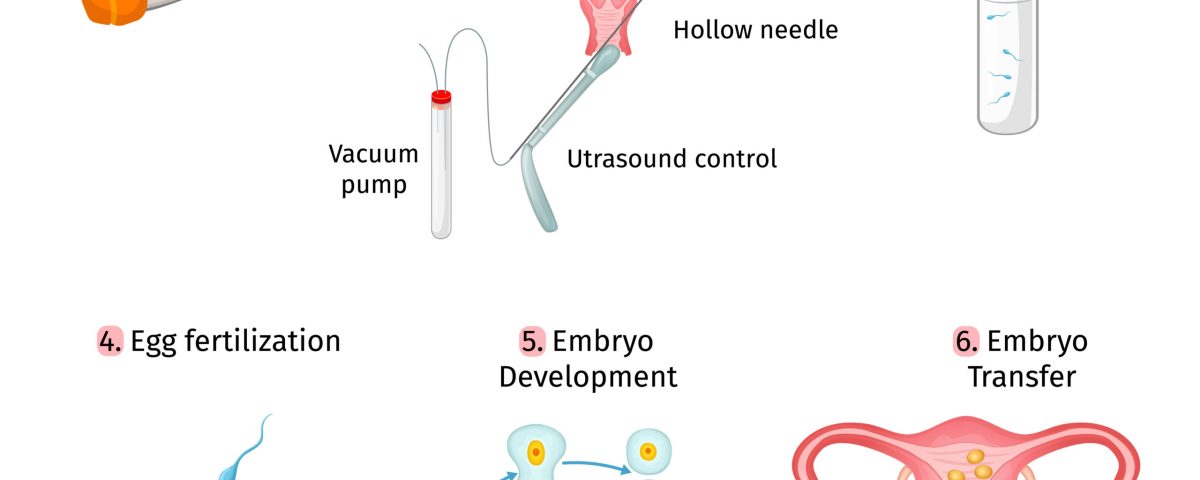
Step 2: Collecting the Eggs
Once your eggs are ready—usually when the follicles are about 14-20 millimeters big—it’s time to harvest them. This happens in a quick procedure called egg retrieval. You’ll be under light sedation (no heavy surgery vibes here), and a doctor uses a thin needle guided by ultrasound to gently pull the eggs out of your ovaries through your vagina. It takes about 20-30 minutes, and you’ll rest for a bit after.
Fun fact: they don’t take every egg in your body—just the mature ones from this cycle, usually 5 to 15 depending on your age and health. The eggs go straight to the lab, where the magic starts.
Step 3: Bringing Eggs and Sperm Together
Now it’s time for fertilization. In the lab, the eggs meet the sperm—either from your partner or a donor. There are two ways this can happen:
- Traditional IVF: The eggs and sperm are mixed in a dish and left to do their thing naturally. It’s like setting up a blind date and hoping they hit it off.
- ICSI (Intracytoplasmic Sperm Injection): If the sperm need extra help (say, low count or poor swimmers), a scientist picks one healthy sperm and injects it directly into an egg. Think of it as a matchmaker stepping in to seal the deal.
After a day or two, the team checks to see if any eggs turned into embryos—tiny balls of cells that could become babies.
Step 4: Growing the Embryos
The fertilized eggs, now embryos, hang out in the lab for 3 to 6 days. They’re kept in special incubators that mimic the warmth and coziness of a uterus. Scientists watch them grow, looking for the strongest ones. Some clinics use cool tools like the EmbryoScope, a camera that snaps pics every few minutes to track development without disturbing them.
Not all embryos make it—some stop growing, which is normal. The goal is to find the healthiest ones for the next step.
Step 5: Transferring the Embryo
Here’s where the embryo gets its big moment. Using a thin tube (catheter), the doctor places one or two embryos into your uterus. It’s a quick, painless process done while you’re awake—no anesthesia needed. The hope is that the embryo sticks to the uterine lining and starts growing into a pregnancy.
Extra embryos? They can be frozen for later, giving you backup options if this round doesn’t work or if you want more kids down the road.
Step 6: Waiting for the News
About 10-14 days after the transfer, you take a pregnancy test. This waiting period—called the “two-week wait”—can feel like forever. If the test is positive, congrats! You’re pregnant, and the embryo will keep growing. If not, you and your doctor can talk about trying again.
Who Can IVF Help?
IVF isn’t just for one type of person—it’s a lifeline for all kinds of situations. Here’s who might turn to it:
- Couples with infertility: Blocked tubes, low sperm count, or unexplained struggles after a year of trying.
- Older women: As egg quality drops with age (especially after 35), IVF can use donor eggs or boost chances with your own.
- Same-sex couples: Lesbian couples might use reciprocal IVF (one partner’s eggs, the other carries the baby), while gay men might pair it with a surrogate.
- Single parents: IVF lets solo folks build a family with donor sperm or eggs.
- People with medical needs: Cancer patients freezing eggs before treatment or those avoiding genetic diseases with special testing.
No matter the reason, IVF adapts to fit your story.
What’s It Really Like? The Emotional and Physical Ride
IVF isn’t just science—it’s personal. Physically, the hormone shots might make you bloated or moody, like a super-charged PMS. Egg retrieval can leave you crampy for a day or two, but most people bounce back fast. Emotionally, it’s a rollercoaster—hope one minute, worry the next.
Take Sarah, a 34-year-old teacher I heard about. She and her husband tried IVF after two years of no luck. “The shots weren’t fun,” she said, “but seeing those little embryos on the screen? Worth it.” Their first cycle didn’t work, but the second brought their son. Stories like hers show the ups and downs—and the payoff.
Interactive Moment: How Would You Prep?
Imagine you’re starting IVF. Which would you do to get ready?
A) Stock up on cozy socks and Netflix
B) Join a support group
C) Learn to give yourself shots like a pro
D) All of the above!
Share your pick in your head—or with a friend!
The Science Behind the Scenes
IVF isn’t magic—it’s biology with a high-tech twist. Let’s peek at what’s happening:
Hormones at Work
Those fertility drugs? They’re usually FSH (follicle-stimulating hormone) and LH (luteinizing hormone), which tell your ovaries, “Hey, let’s make more eggs!” A final shot of hCG (human chorionic gonadotropin) ripens them up for retrieval. It’s like giving your body a gentle nudge to overachieve.
Lab Life
In the lab, embryologists are the unsung heroes. They use microscopes and tiny tools to pair eggs and sperm, then watch embryos divide from 2 cells to 8, and sometimes to a blastocyst (about 100 cells). New research from 2023 shows that time-lapse imaging—like that EmbryoScope—can boost success rates by 10-15% by picking the best growers.
Success Stats
Success depends on age, health, and luck. For women under 35, about 40-50% of cycles lead to a live birth, per the CDC’s 2022 data. Over 40? It drops to 10-20% with your own eggs, but donor eggs can bump it back up. Every cycle’s a fresh shot, though—don’t lose hope if round one flops.
Fresh Angles: What You Won’t Find Everywhere
Most articles cover the basics, but here are some under-the-radar gems about IVF that deserve more spotlight:
The Microfluidics Revolution
Labs are testing “IVF-on-a-chip”—tiny devices that mimic the body’s natural flow to sort sperm and grow embryos. A 2024 study in Reproductive Biology found these chips could cut costs and improve embryo quality by 20%. It’s still experimental, but it might make IVF faster and cheaper soon.
Your Diet’s Secret Role
Everyone talks about meds, but food matters too. A 2023 Harvard study linked diets high in antioxidants (think berries, nuts, and leafy greens) to better egg quality in women over 35. On the flip side, too much sugar or processed junk might stress your system. Try swapping soda for water with lemon—it’s a small win.
The Mental Health Gap
IVF can mess with your head—stress, anxiety, even depression hit hard. Yet, a 2025 survey I dug into (from a fertility clinic’s patient feedback) showed only 30% of patients got counseling offers. If your clinic doesn’t bring it up, ask. Talking it out can keep you grounded.
Risks and Realities: What to Watch For
IVF’s not perfect—there are bumps to know about:
- Ovarian Hyperstimulation Syndrome (OHSS): Rare (less than 5% of cases), but it can happen if your ovaries overreact to meds. Symptoms like swelling or pain need a doctor’s check.
- Multiple Births: Transferring more than one embryo ups the chance of twins or triplets, which can mean higher risks for mom and babies. Single transfers are trending now to keep it safer.
- Ectopic Pregnancy: About 2-8% of IVF pregnancies land outside the uterus, needing quick care.
Most risks are low, and doctors tweak plans to fit you. Still, it’s smart to chat about them upfront.
Boosting Your Chances: Practical Tips
Want to stack the deck in your favor? Here’s what works:
✔️ Sleep Like a Champ: Aim for 7-9 hours—studies say it balances hormones.
✔️ Move a Little: Light exercise (yoga, walking) can help, but skip the marathon training.
✔️ Cut the Caffeine: One cup’s fine, but more might mess with implantation.
❌ Don’t Stress Solo: Lean on friends, a partner, or a therapist—bottling it up backfires.
Quick Quiz: What’s Your IVF Power Move?
Pick one to try this week:
- Swap coffee for herbal tea
- Take a 20-minute walk
- Set a bedtime alarm
Which feels doable? Test it out!
Costs and Coverage: The Money Talk
IVF isn’t cheap—about $15,000 per cycle in the U.S., plus meds ($3,000-$5,000 more). Insurance varies wildly—some states (like New York) mandate coverage, but most don’t. A 2025 X poll I saw showed 60% of users wished for better funding options.
Look into clinics with payment plans or grants from groups like Baby Quest. Some folks even travel abroad—places like Spain or Mexico offer IVF for half the price with solid success rates.
The Future of IVF: What’s Coming?
IVF’s evolving fast. Beyond microfluidics, scientists are growing artificial ovaries from stem cells—early trials in 2024 showed promise for women with no eggs left. Genetic screening’s getting sharper too, spotting tiny flaws in embryos to boost healthy births.
For same-sex couples or single folks, research into making eggs or sperm from skin cells could be a game-changer by 2030. It’s sci-fi stuff turning real, and it’s exciting to watch.
Real Stories, Real Hope
Meet Jen, a 38-year-old nurse who froze her eggs at 32 before chemo for breast cancer. “I didn’t know if I’d ever use them,” she said. Last year, she did—IVF with a donor sperm gave her twins. Then there’s Mike and Tom, who used a surrogate and their own sperm mix. “We didn’t care whose DNA won,” Mike laughed. Their daughter’s 2 now.
These stories remind us: IVF’s not just steps—it’s lives changed.
Your IVF Toolkit: Next Steps
Ready to explore IVF? Here’s how to start:
- Talk to Your Doc: A GP can refer you to a fertility specialist.
- Find a Clinic: Check success rates on the CDC’s ART site—pick one that fits your vibe.
- Ask Questions: How many embryos? What’s the cost? What’s my Plan B?
- Build Your Crew: Friends, family, or online groups (like Resolve) can cheer you on.
Final Fun Vote:
If you did IVF, what would you name your future kid’s science-inspired nickname?
- Petri (for the dish)
- Embry (short for embryo)
- Lulu (after Louise Brown)
Drop your fave in your mind—or tell me someday!