How Much Is IVF Without Insurance?
April 17, 2025
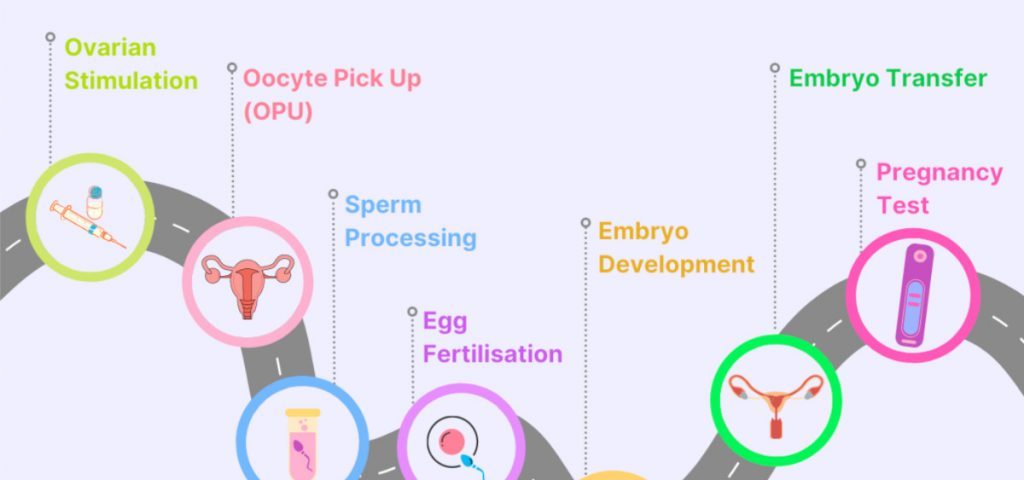
How IVF Works: A Step-by-Step Guide to Your Fertility Journey
April 17, 2025How Does IVF Work? A Step-by-Step Guide to In Vitro Fertilization
In vitro fertilization, or IVF, is like a superhero for people dreaming of starting a family but facing roadblocks. It’s a process that takes science, hope, and a little bit of patience to help create life outside the body before bringing it back in. If you’ve ever wondered what happens behind the scenes of this incredible journey, you’re in the right place. This guide will walk you through every step, sprinkle in some science, and share practical tips—plus a few things you might not find anywhere else. Whether you’re curious, considering IVF, or supporting someone who is, let’s dive into this amazing world together.
What Is IVF, Anyway?
IVF stands for “in vitro fertilization,” which is just a fancy way of saying “fertilization in glass.” Picture a lab where eggs and sperm meet up in a petri dish instead of inside the body. It’s part of a bigger group of tools called assisted reproductive technology (ART), designed to help people who can’t conceive naturally. Since the first IVF baby, Louise Brown, was born in 1978, over 8 million babies worldwide have come into the world this way. Pretty cool, right?
IVF isn’t just for one type of person. It helps women with blocked fallopian tubes, men with low sperm counts, same-sex couples, or even single folks wanting to become parents. It’s like a bridge between dreams and reality, and it all starts with a carefully planned process.
Step 1: Boosting Egg Production with Ovarian Stimulation
The IVF journey kicks off with a boost to the ovaries. Normally, your body releases one egg a month during ovulation, but IVF needs more to work with. Doctors prescribe fertility drugs—usually injections you give yourself at home—to encourage your ovaries to produce several eggs at once. Think of it like giving your ovaries a pep talk to step up their game.
These medications, like follicle-stimulating hormone (FSH), mimic your body’s natural signals. Over about 8-14 days, they help multiple follicles (tiny sacs where eggs grow) mature. You’ll visit the clinic for ultrasounds and blood tests to check hormone levels and see how those eggs are coming along. The goal? To get a handful of healthy eggs ready for the next step.
What’s It Like?
- The Good: More eggs mean better chances of success.
- The Tricky: You might feel bloated, moody, or tired from the hormones. Some folks even get a rare condition called ovarian hyperstimulation syndrome (OHSS), where the ovaries overreact, but doctors keep a close eye to prevent it.
Pro Tip
Start a mini journal to track how you feel each day. It’ll help you spot patterns and give your doctor useful info if something feels off.
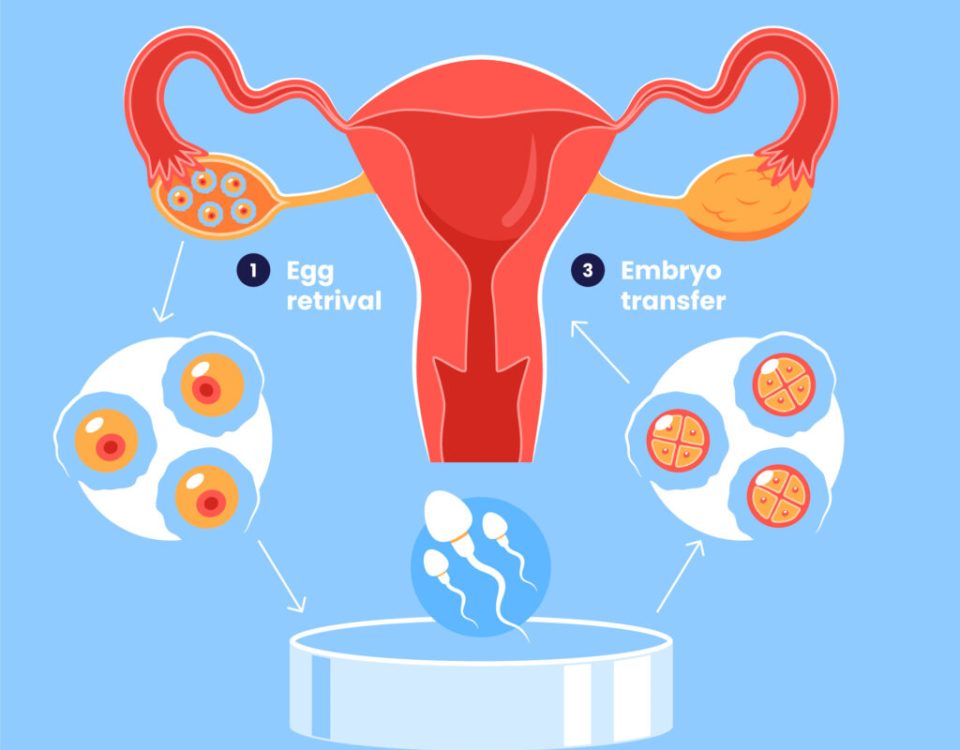
Step 2: Egg Retrieval—Harvesting the Goods
Once your eggs are ready—usually when the follicles hit about 18-20 millimeters— it’s time for egg retrieval. This happens around day 12-14 of your cycle. You’ll get a trigger shot (a hormone like hCG) to ripen those eggs, and about 36 hours later, you’re in the clinic.
Here’s how it goes: You’re lightly sedated (no heavy anesthesia needed), and a doctor uses an ultrasound-guided needle to gently pull the eggs out of your ovaries through the vaginal wall. It takes about 20-30 minutes, and you’ll rest for a bit after. Most people go home the same day with 5-15 eggs in tow, depending on age and response to the meds.
Fun Fact
The needle is super thin—about the width of a paperclip—so it’s less scary than it sounds. Plus, you’re asleep for the whole thing!
Watch Out For
- ✔️ Mild cramping or spotting? Totally normal.
- ❌ Severe pain or heavy bleeding? Call your doctor ASAP.
Step 3: Sperm Collection and Fertilization
While your eggs are being retrieved, your partner (or a donor) provides a sperm sample. The lab team washes and preps the sperm to pick out the healthiest swimmers. Then, it’s showtime: eggs and sperm meet in the lab.
There are two ways this can happen:
- Traditional IVF: Sperm and eggs are mixed in a dish, and nature takes its course. About 60-70% of eggs fertilize this way if sperm quality is good.
- ICSI (Intracytoplasmic Sperm Injection): If sperm count or movement is low, a single sperm is injected right into an egg with a tiny needle. This boosts the odds when things are tricky.
After 18-24 hours, the lab checks to see if fertilization worked. If it did, those fertilized eggs—now called embryos—start growing.
A Peek at the Science
A 2023 study from the American Society for Reproductive Medicine found ICSI ups success rates by 10-15% in cases of male infertility. It’s like giving the sperm a VIP pass to the egg!
Couple’s Corner
For same-sex female couples, reciprocal IVF is an option. One partner donates the eggs, and the other carries the pregnancy—sharing the journey in a unique way.
Step 4: Embryo Development—Growing Tiny Miracles
For the next 3-6 days, the embryos chill in an incubator that mimics the womb’s cozy environment. Lab experts watch them divide and grow, grading their quality. By day 5 or 6, the best ones reach the blastocyst stage—a ball of about 100 cells ready to implant.
Not all embryos make it this far, and that’s okay—it’s part of the process. The strongest ones are picked for transfer, and extras can be frozen for later.
What Makes a Good Embryo?
- Size and shape of cells
- How evenly they divide
- No weird fragments
Interactive Quiz: How Many Embryos Survive?
Guess how many eggs typically turn into blastocysts:
- A) 80-90%
- B) 50-60%
- C) 20-30%
(Answer: B! About half make it, depending on age and health.)
Step 5: Embryo Transfer—Planting the Seed
Now comes the big moment: transferring an embryo into the uterus. It’s a quick, painless procedure—no sedation needed. The doctor threads a thin catheter through your cervix and places the embryo (or sometimes two) into your womb, guided by ultrasound. You’ll lie down for a bit after, then head home.
Timing is everything here. Fresh transfers happen 3-5 days after retrieval, but frozen embryo transfers (FET) are more common now. Why? Freezing lets your body recover from the hormones, and a 2024 study from Yale showed FET boosts live birth rates by 5-10% in women over 35.
Fresh vs. Frozen: A Quick Breakdown
| Type | Pros | Cons |
|---|---|---|
| Fresh Transfer | Faster process | Hormones might affect lining |
| Frozen Transfer | Better uterine prep | Extra wait time |
Aftercare Tip
Rest, but don’t overdo it. Light walks are fine—your embryo won’t “fall out” (a common myth!).
Step 6: The Two-Week Wait and Pregnancy Test
The next 10-14 days are the infamous “two-week wait.” The embryo needs to implant in your uterine lining, and there’s not much to do but stay calm and hopeful. Around day 12-14 post-transfer, you’ll take a blood test at the clinic to check for pregnancy hormones (hCG).
How to Survive the Wait
- ✔️ Distract yourself with a new hobby—painting, anyone?
- ❌ Don’t test early at home; it could give a false result and mess with your emotions.
Success Stats
For women under 35, about 50% of transfers lead to a live birth, per 2021 data from the Society for Assisted Reproductive Technology. Over 40? It drops to 7-10%, but every case is unique.
What Happens If It Works—or Doesn’t?
If the test is positive, congrats—you’re pregnant! You’ll start prenatal care, and the clinic will monitor you for a few weeks. If it’s negative, it’s tough, but not the end. Many people need 2-3 cycles to succeed. Your doctor will tweak the plan based on what happened—like adjusting meds or trying a frozen transfer.
A Real Story
Take Sarah, a 38-year-old teacher from Iowa. After two failed cycles, her team switched to a lower-dose protocol and used a frozen transfer. Third time was the charm—she’s now mom to a spunky toddler.
The Costs and Emotional Rollercoaster
IVF isn’t cheap—$12,000-$25,000 per cycle in the U.S., and insurance doesn’t always cover it. But there’s hope: some states mandate coverage, and clinics offer payment plans. Emotionally, it’s a wild ride. The highs of a positive test and lows of a negative can hit hard.
Money-Saving Hacks
- Check for grants from groups like BabyQuest.
- Ask about multi-cycle discounts—some clinics cut costs if you commit to a package.
Emotional Support
Join an online group or see a counselor who gets IVF. You’re not alone in this.
Risks and Realities You Should Know
IVF is safe, but not risk-free. Multiple pregnancies (twins or more) happen in 20-30% of cases if two embryos are transferred, raising risks like preterm birth. There’s also a 2-5% chance of an ectopic pregnancy, where the embryo implants outside the uterus. And those fertility drugs? They can cause bloating or, rarely, OHSS.
Minimizing Risks
- Opt for single embryo transfer (SET)—it’s safer and just as effective for most.
- Watch for signs like severe abdominal pain and report them fast.
New Twists: What’s Hot in IVF Today
IVF keeps evolving, and 2025 brings fresh ideas. Here are three things you won’t find in every article:
1. Coenzyme Q10 for Older Eggs
Research from the University of Toronto (2017, updated 2023) shows CoQ10 supplements might improve egg quality in women over 35. It’s an antioxidant that boosts mitochondrial energy in eggs, potentially cutting aneuploidy (chromosome issues) by up to 15%. Ask your doc about adding 200-600 mg daily before your cycle.
2. AI Picking the Best Embryos
Labs are testing artificial intelligence to analyze embryo images and predict which ones will thrive. A 2024 trial at NYU Langone saw a 12% bump in success rates. It’s not everywhere yet, but it’s a game-changer on the horizon.
3. Microfluidics: The Future Lab-on-a-Chip
Imagine an IVF lab shrunk onto a tiny chip. Microfluidics automates egg and sperm handling, cutting human error. A 2022 Cureus review says it’s still experimental, but early tests show higher fertilization rates. Watch this space!
Your IVF Action Plan
Ready to explore IVF? Here’s a step-by-step guide to get started:
- Find a Clinic: Look for one with high success rates (check SART.org) and a vibe you like.
- Meet the Team: Ask about their approach—do they customize plans? What’s their FET success like?
- Prep Your Body: Eat well, cut stress, and consider CoQ10 if you’re over 35.
- Plan the Cash: Save up, research grants, or check insurance in states like California or New York.
- Build a Crew: Line up friends, family, or a support group to cheer you on.
Quick Poll: What’s Your Biggest IVF Question?
- A) How much will it cost me?
- B) What are my real chances?
- C) How do I stay sane during this?
(Share your pick in your head—or with a friend!)
Wrapping It Up: IVF Is a Journey, Not a Race
IVF is a blend of science, grit, and a sprinkle of magic. It’s not a straight shot—there are twists, turns, and sometimes detours—but it’s opened doors for millions. Whether it’s boosting egg numbers, picking the perfect embryo, or riding out the wait, every step brings you closer to your goal. And with new tricks like AI and microfluidics, the future’s looking bright.
So, if you’re thinking about IVF, take it one day at a time. Talk to experts, lean on your people, and keep hope alive. You’ve got this—and science has your back.