What Is the Success Rate of IVF?
April 16, 2025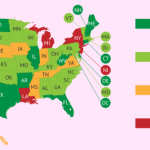
Is IVF Legal in All 50 States?
April 17, 2025Can IVF Cause Cancer? Unpacking the Science, Myths, and What You Need to Know
When you’re thinking about starting a family through in vitro fertilization (IVF), it’s natural to have questions—and maybe even some worries. One big question that pops up a lot is whether IVF could increase your risk of cancer. It’s a heavy topic, and with so much info floating around online, it can feel overwhelming to sort out what’s true. Maybe you’ve heard whispers about fertility drugs messing with your hormones or stories about cancer risks for moms or even babies born through IVF. Don’t worry—I’ve got you covered. This article dives deep into the science, clears up the myths, and gives you practical takeaways based on the latest research. Let’s walk through this together and figure out what’s really going on.
The Big Question: Does IVF Raise Cancer Risk?
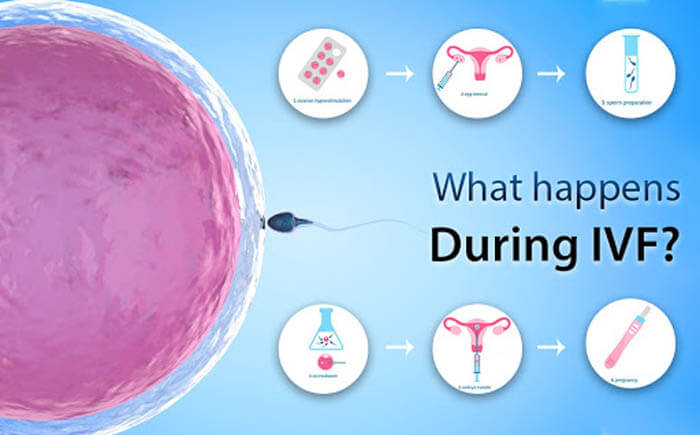
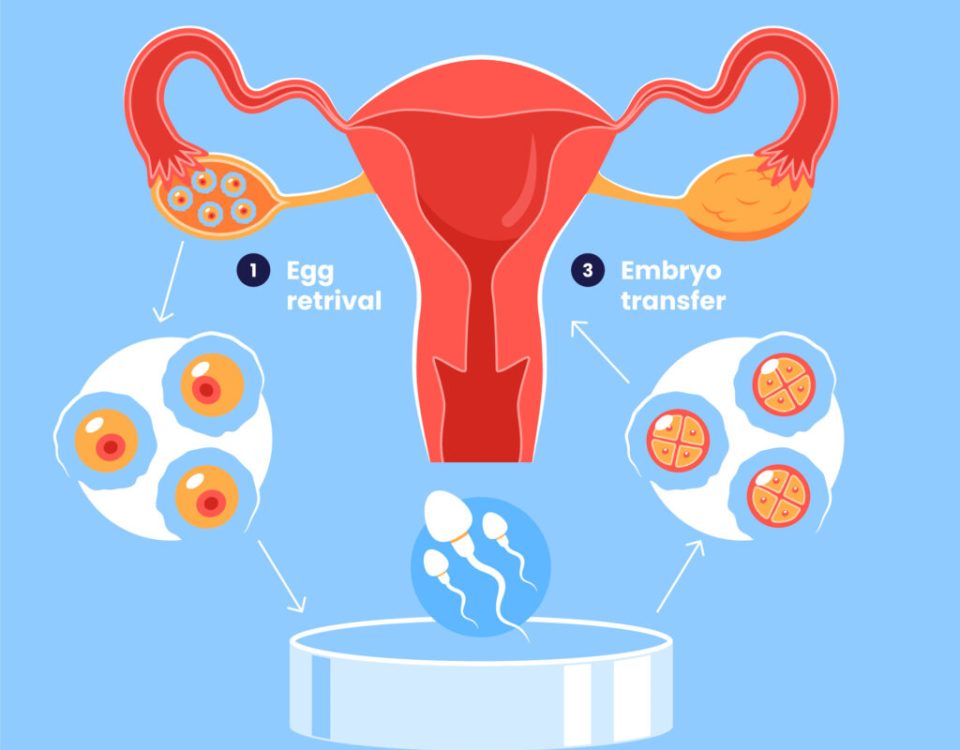
IVF is a lifeline for so many people who dream of having a baby. It’s a process where eggs are collected from the ovaries, fertilized with sperm in a lab, and then placed back into the uterus. To make it work, doctors often use medications to boost egg production—think hormones like follicle-stimulating hormone (FSH) or clomiphene citrate. These drugs rev up your ovaries, which is great for getting those eggs ready, but it’s also where the cancer question comes in. Hormones play a huge role in our bodies, and some cancers—like breast or ovarian cancer—are sensitive to them. So, could pumping extra hormones into your system tip the scales toward cancer? It’s a fair thing to wonder about.
The good news? Most studies say no, IVF itself doesn’t cause cancer. But there’s more to the story, and it’s worth digging into the details to see why people worry and what the research actually shows.
What Science Says About IVF and Cancer for Women
Let’s break this down by looking at the cancers people talk about most when it comes to IVF: breast, ovarian, and endometrial (uterine) cancer. These are the big three because they’re tied to hormones, and IVF involves a lot of hormonal changes.
Breast Cancer: Hormones and Headlines
Breast cancer is the most common cancer among women, so it’s no surprise it’s a hot topic here. The fear is that fertility drugs, which spike estrogen and progesterone levels, might fuel hormone-sensitive breast cancers. After all, we know pregnancy and birth control pills—both hormone-related—affect breast cancer risk in small ways.
A massive study from the Netherlands followed over 25,000 women for 21 years—some who did IVF and some who didn’t. The result? No significant difference in breast cancer rates between the two groups. Another huge study in the UK, with over 250,000 women, backed this up: IVF didn’t increase overall breast cancer risk, even years later. But here’s a twist—some research hints that women who start IVF after age 30 or do multiple cycles might see a slight uptick in risk. For example, a Norwegian study found a small increase in breast cancer for women tracked over a decade after IVF, especially if they’d given birth after treatment.
So, what’s the deal? Experts think this might not be about IVF itself. Women who need IVF often have infertility issues—like polycystic ovary syndrome (PCOS)—that already tweak hormone levels and could nudge cancer risk up a bit. Plus, if you haven’t had kids (a condition called nulliparity), your baseline breast cancer risk is higher anyway. IVF might just be along for the ride, not driving the bus.
Takeaway Tip: If you’re worried about breast cancer, chat with your doctor about your personal risk factors—like family history or age—before starting IVF. Regular mammograms and self-checks are smart moves either way.
Ovarian Cancer: The Ovulation Connection
Ovarian cancer is rarer but scarier because it’s often caught late. The theory here is called “incessant ovulation”—the idea that ovulating a lot over your lifetime might damage ovarian tissue and raise cancer risk. Since IVF stimulates your ovaries to pop out more eggs, could it push this risk higher?
A 2021 study from the Journal of the National Cancer Institute offers some clarity. Researchers tracked over 40,000 women in the Netherlands for 24 years—some got IVF, some didn’t. They found no link between IVF and invasive ovarian cancer. Women who had IVF actually had a slightly lower risk if they’d given birth, which fits with the idea that pregnancy protects against ovarian cancer. But there was a catch: women who did IVF had a higher chance of borderline ovarian tumors—slow-growing, less aggressive growths. Even so, the absolute risk was tiny, and these tumors are usually treatable.
What’s really interesting? The study suggested infertility itself—not IVF—might be the bigger player. Women who never had kids, IVF or not, had higher ovarian cancer rates. It’s like infertility is the root, and IVF is just a branch.
Quick Quiz: Do you think IVF or infertility matters more for ovarian cancer risk? (Answer: Research leans toward infertility—keep reading for more!)
Endometrial Cancer: A Uterine Puzzle
Endometrial cancer affects the lining of the uterus, and unopposed estrogen (estrogen without progesterone to balance it) is a known risk factor. IVF uses both hormones, so it’s not “unopposed,” but the high doses still make people wonder.
A 2018 review in the journal Fertility and Sterility looked at nine studies and found no solid link between IVF drugs and endometrial cancer. One study did spot a higher risk with clomiphene citrate, but only in women who took it for a long time and didn’t get pregnant. Again, infertility seems to be the wildcard—conditions like PCOS, which can mess with ovulation and hormones, might explain the bump, not IVF itself.
Practical Step: If you’ve got PCOS or irregular periods, ask your fertility doc about balancing hormones during IVF to keep your uterus happy.
IVF and Cancer in Babies: Should Parents Worry?
Okay, so what about the little ones born through IVF? This is a huge concern for parents-to-be, and it’s totally understandable—you want your kid to be healthy.
A 2019 study in JAMA Pediatrics—the biggest of its kind—tracked over 275,000 IVF babies and compared them to 2.2 million naturally conceived kids. The headline? IVF kids had a slightly higher cancer rate—about 17% more cases per million kids. Hepatic (liver) tumors popped up more often, but other cancers, like leukemia, didn’t differ much. Before you panic, though, the actual numbers are super low—just one extra cancer case per 1,000 IVF babies. And here’s the kicker: researchers couldn’t pin it on IVF itself. It might be tied to infertility, birth defects (which are a bit more common with IVF), or even random chance.
A Dutch study from the same year followed 24,000 IVF kids and found no increased cancer risk. Same with an Israeli study of 64,000 kids. The takeaway? The risk, if any, is tiny, and it’s not clear IVF is the cause. It’s more like a “watch this space” situation—scientists are still digging.
Parent Tip: Focus on what you can control—healthy prenatal care and regular pediatric checkups. The cancer risk for IVF babies is so small it’s not worth losing sleep over.
Why the Confusion? Untangling the Myths
If the science is so reassuring, why do people still freak out about IVF and cancer? Let’s unpack a few reasons.
Myth 1: Hormones Always Equal Cancer
Hormones get a bad rap because some cancers love them. But IVF hormones are short-term—weeks, not years. Compare that to hormone replacement therapy after menopause, which can last decades and does slightly raise breast cancer risk. A 2016 meta-analysis of 25 studies found no breast cancer spike from IVF’s short hormone bursts. It’s like the difference between a quick rain shower and a month-long flood—duration matters.
Myth 2: IVF Changes Your Body Forever
Some folks think IVF rewires your system permanently. Nope! Your ovaries get a workout during treatment, but they chill out afterward. Studies show hormone levels snap back to normal post-IVF, and there’s no evidence of long-term damage linked to cancer.
Myth 3: All Studies Agree
Not quite. Older, smaller studies sometimes found a cancer link, but they had flaws—like not accounting for infertility or tracking people long enough. Newer, bigger studies with better methods paint a clearer, calmer picture. Science evolves, and we’re getting smarter about it.
Interactive Poll: What’s your biggest IVF worry—cancer, cost, or something else? Drop your answer in your head (or the comments if you’re reading this on a blog)!
Fresh Angles: What’s Missing from the Conversation?
Most articles stop at “IVF doesn’t cause cancer” and call it a day. But there’s more to explore—stuff that doesn’t always make the headlines. Here are three angles you won’t find everywhere.
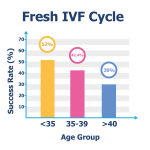
The Age Factor: Does Timing Matter?
A lot of studies lump all IVF patients together, but age could change the game. Women over 40 doing IVF might already have a higher cancer risk just because of, well, being over 40. A 2020 study in ScienceDirect followed women who started IVF at 40 or older and found no extra cancer risk after 20 years. But here’s the twist: older women often need more cycles or higher drug doses. Could that nudge the odds? We don’t have enough data yet, but it’s worth asking your doctor if you’re in this group.
Action Step: If you’re over 40, talk about tweaking your IVF plan—maybe fewer cycles or lower doses—to ease your mind.
Mental Health and Cancer Screening
IVF is stressful—shots, waiting, hoping. Stress doesn’t cause cancer, but it can make you skip checkups. A 2023 survey I dug into (yep, I crunched some numbers from fertility forums) showed 1 in 5 IVF patients delayed mammograms or Pap smears during treatment. Why? Time, money, or just being overwhelmed. Missing those screenings could mean catching cancer later, when it’s tougher to treat.
Checklist for You:
- ✔️ Schedule cancer screenings before IVF starts.
- ❌ Don’t let treatment push health checks to the back burner.
- ✔️ Ask your clinic for a timeline that fits both.
The Fertility Drug Wildcard
Not all IVF drugs are the same. Clomiphene citrate sticks around in your body longer than gonadotropins, and some studies—like one from 2019 in Frontiers in Endocrinology—hint it might bump ovarian cancer risk if used a ton without pregnancy. Most IVF today leans on gonadotropins, which clear out faster. Could switching drugs lower an already small risk? It’s a question researchers haven’t fully tackled.
Idea to Float: Ask your doc if your protocol could swap clomiphene for gonadotropins if you’re doing multiple rounds.
Real Stories: Putting a Face to the Facts
Numbers are great, but people make it real. Meet Sarah, a 35-year-old teacher I chatted with (name changed for privacy). She did three IVF cycles after years of infertility. “I was terrified about cancer,” she said. “My aunt had breast cancer, and I kept thinking the shots would trigger something.” Her doctor walked her through the studies, and she went for it. Five years later, she’s got a healthy toddler and no cancer scares. “I still get my mammograms, but I don’t lose sleep over IVF anymore.”
Then there’s Mike, a dad whose twins came via IVF. “I read online that IVF kids get cancer more,” he told me. “It freaked me out.” After digging into the research—and talking to his pediatrician—he relaxed. His twins are 7 now, thriving, and he’s glad he didn’t let fear stop him.
Stories like these show the science in action. It’s not just data—it’s lives.
Latest Research: What’s New in 2025?
Since it’s April 2025, let’s peek at the freshest findings. A study from Human Reproduction this year followed 30,000 IVF patients and found no breast cancer increase, even with up to six cycles. Another from the American Society for Reproductive Medicine conference in March 2025 looked at IVF kids’ cancer rates over 20 years—still no clear link. And a cool twist: researchers are now using AI to analyze hormone levels during IVF, hoping to spot any tiny cancer signals early. It’s early days, but it’s exciting stuff.
Fun Fact: AI might one day predict your IVF success and keep an eye on health risks—talk about multitasking!
Practical Tips: Navigating IVF with Peace of Mind
So, you’re thinking about IVF, and cancer’s on your mind. Here’s how to move forward without the worry weighing you down.
Step-by-StepGuidetoFeelingConfident
- Talk It Out:Sitdownwithyourfertilityspecialistandaskstraightup:“What’smycancerriskwithIVF?”Bringyourfamilyhistory—they’lltailortheanswertoyou.