Why Are Republicans Against IVF? Exploring the Debate
April 16, 2025
What Insurance Covers IVF: Your Guide to Fertility Treatment Coverage
April 16, 2025What Is IVF? Your Complete Guide to In Vitro Fertilization
In vitro fertilization, or IVF, is a term you might’ve heard tossed around in conversations about starting a family, especially when things don’t go as planned naturally. Maybe you’ve seen it in a movie, read about it in a magazine, or even know someone who’s gone through it. But what exactly is IVF? How does it work, and why do people turn to it? If you’re curious about this life-changing process, you’re in the right place. This guide is here to break it all down for you—think of it as your friendly, no-nonsense roadmap to understanding IVF from start to finish.
IVF isn’t just a medical procedure; it’s a journey filled with hope, science, and sometimes a few surprises. Whether you’re exploring it for yourself or just want to know more, we’ll cover the basics, dive into the details, and even touch on some things you won’t find in every article—like how it feels emotionally, what the latest research says, and tips to make the process smoother. So, grab a comfy seat, and let’s dive into the world of IVF together!
The Basics: What Does IVF Mean?
IVF stands for in vitro fertilization. That’s a fancy way of saying “fertilization in a lab.” In simple terms, it’s a process where doctors take an egg from a woman and sperm from a man, combine them outside the body in a lab dish, and then place the resulting embryo back into the woman’s uterus to grow into a baby. The “in vitro” part comes from Latin, meaning “in glass,” because it happens in a petri dish—not inside the body like natural conception.
This isn’t something new—IVF has been around since 1978 when the first “test-tube baby,” Louise Brown, was born in England. Since then, millions of babies have come into the world thanks to this technology. It’s a big deal for people who can’t get pregnant the usual way, whether because of blocked tubes, low sperm count, or other challenges.
So, who uses IVF? It’s not just for one type of person. Couples with infertility, single parents, same-sex couples, and even people wanting to avoid passing on genetic conditions might choose it. It’s like a helping hand from science when nature needs a boost.
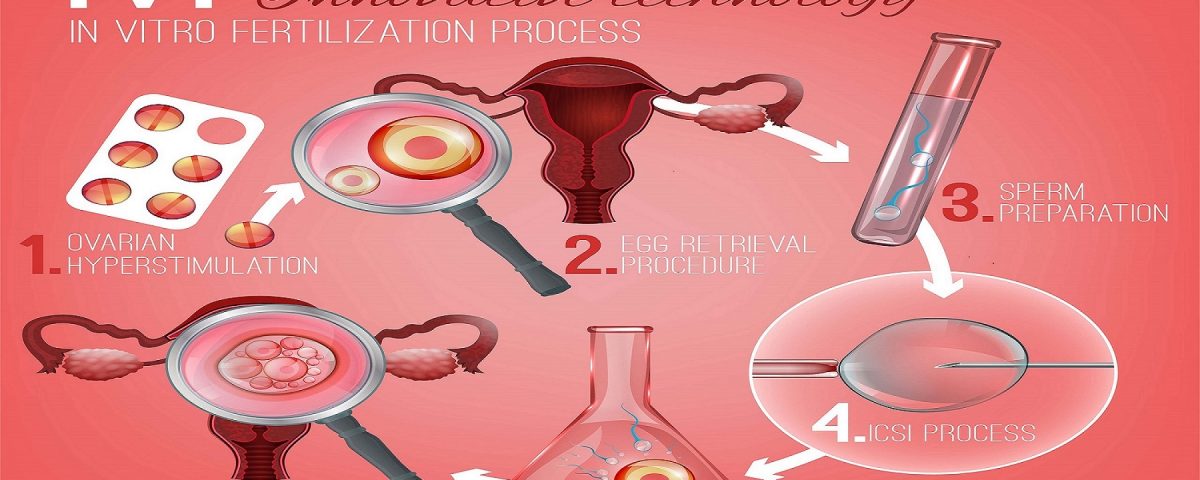
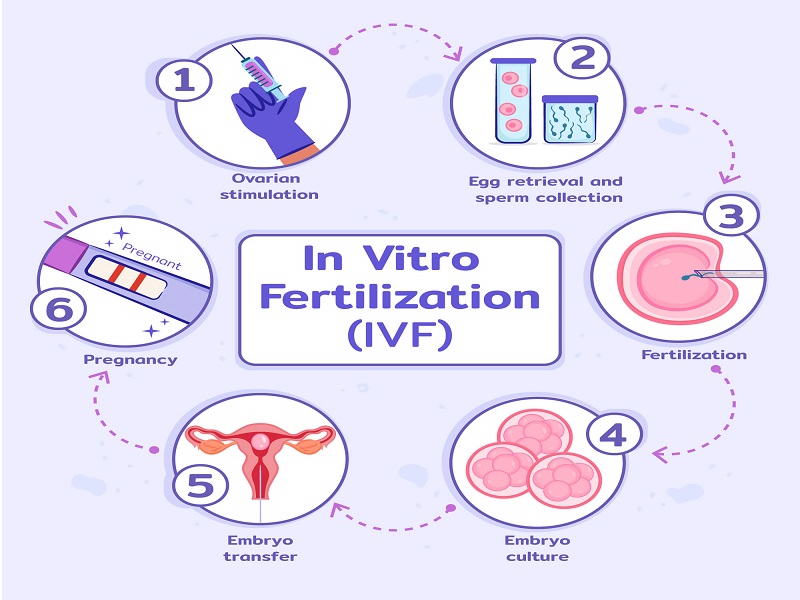
How Does IVF Work? A Step-by-Step Look
IVF isn’t a one-and-done thing—it’s a series of steps that can take weeks or even months. Each part is carefully planned to give the best shot at success. Here’s how it usually goes:
Step 1: Boosting Egg Production
First, a woman takes special medicines called fertility drugs. Normally, your ovaries release one egg a month, but these drugs tell them to make several at once. More eggs mean more chances for a healthy embryo. You’ll get shots or pills for about 10-14 days, and doctors will check your progress with blood tests and ultrasounds.
✔️ Tip: Keep a small journal to track how you feel—some people get bloating or mood swings from the meds.
❌ Don’t: Skip doses; timing is everything here!
Step 2: Collecting the Eggs
Once the eggs are ready, a doctor uses a thin needle to gently remove them from the ovaries. This happens under light anesthesia, so you won’t feel much. It’s quick—about 20 minutes—and you’ll rest afterward. The eggs go straight to the lab.
Step 3: Bringing Sperm and Egg Together
Next, the sperm (from a partner or donor) meets the eggs. In traditional IVF, they’re mixed in a dish and left to fertilize naturally. If sperm quality is low, doctors might use a technique called ICSI (intracytoplasmic sperm injection), where they inject a single sperm directly into an egg. Either way, the goal is to create embryos.
Step 4: Growing the Embryos
The fertilized eggs—now embryos—spend a few days growing in the lab. Scientists watch them closely, usually for 3-5 days, to see which ones look strongest. This part feels like a waiting game, but it’s crucial.
Step 5: Placing the Embryo in the Uterus
Finally, one or two healthy embryos are transferred into the woman’s uterus using a thin tube. It’s painless and takes just a few minutes. If all goes well, the embryo implants in the uterine lining, and pregnancy begins. About two weeks later, a test confirms if it worked.
Fun Fact: Extra embryos can be frozen for later—think of it like saving a backup plan!
Why People Choose IVF: More Than Just Infertility
IVF isn’t only for couples who can’t conceive naturally. It’s a tool with lots of uses, depending on someone’s situation. Here are some common reasons people turn to it:
- Blocked or Damaged Fallopian Tubes: If the tubes that carry eggs to the uterus are blocked, sperm can’t reach the egg naturally. IVF skips that step entirely.
- Low Sperm Count or Quality: When sperm can’t do the job on their own, IVF (especially with ICSI) gives them a direct path to the egg.
- Age-Related Challenges: As women get older, egg quality drops. IVF can use younger, healthier eggs (sometimes from a donor) to boost chances.
- Genetic Concerns: Some people use IVF with genetic testing to avoid passing on conditions like cystic fibrosis.
- Fertility Preservation: Cancer patients or those delaying parenthood might freeze eggs or embryos for later use.
It’s not just about biology, either. Single folks and same-sex couples often use IVF with donor sperm, eggs, or surrogates to build their families. It’s a flexible option that’s opened doors for all kinds of people.
What’s It Really Like? The Emotional Side of IVF
Let’s be real—IVF isn’t just needles and lab dishes. It’s an emotional rollercoaster, too. One day you’re hopeful, the next you’re stressed about results. Studies show that up to 40% of people going through IVF feel anxious or down at some point. That’s normal—it’s a big deal!
Take Sarah, a 32-year-old teacher I heard about. She and her husband tried IVF after years of struggling. “The waiting was the hardest,” she said. “Every test felt like a make-or-break moment.” They celebrated small wins, like a good embryo, but also faced setbacks when a cycle didn’t work. Eventually, they had a daughter—and said it was worth every tear.
Here’s a quick checklist to help you cope:
✔️ Talk to someone—a friend, therapist, or support group can lighten the load.
✔️ Take breaks when you need them; it’s okay to step back and breathe.
❌ Don’t bottle it up—ignoring your feelings can make it tougher.
The Science Behind IVF: What’s New in 2025?
IVF isn’t stuck in the past—it’s always evolving. By April 2025, researchers have made some cool advances that are changing the game. Here’s what’s fresh:
Better Embryo Selection
Labs now use AI to pick the best embryos. A 2024 study from the University of California found that AI tools boosted success rates by 15% compared to human judgment alone. It’s like having a super-smart assistant in the lab!
Lab-on-a-Chip Technology
This tiny device mimics the body’s natural environment for eggs and sperm. It’s still experimental, but early tests show it could make fertilization more efficient. Think of it as a mini science lab in your pocket.
In Vitro Gametogenesis (IVG)
This is wild—scientists are working on turning skin cells into eggs or sperm. It’s not ready yet, but a 2025 report from Reproductive Sciences says it could help people who can’t produce gametes naturally. Imagine growing your own eggs from scratch!
These breakthroughs aren’t in every clinic yet, but they’re hints of where IVF is headed. Staying updated can help you ask your doctor about cutting-edge options.
How Much Does IVF Cost—and Can You Afford It?
IVF isn’t cheap. In the U.S., one cycle averages $15,000-$20,000, and many people need more than one try. Insurance doesn’t always cover it—only about 20 states require some coverage. Add in meds ($3,000-$5,000) and extras like genetic testing, and it piles up fast.
But there are ways to make it work:
- Grants and Discounts: Groups like Baby Quest offer financial help. Some clinics have sliding-scale fees based on income.
- Employer Benefits: Big companies like Google and Starbucks now cover IVF for employees. Check your job’s perks!
- Payment Plans: Many clinics let you pay over time, easing the upfront hit.
Here’s a quick table to give you a sense of costs:
| Item | Average Cost | Notes |
|---|---|---|
| IVF Cycle | $15,000-$20,000 | Includes basic procedure |
| Medications | $3,000-$5,000 | Varies by dose |
| Genetic Testing | $2,000-$4,000 | Optional but common |
| Frozen Embryo Transfer | $3,000-$5,000 | For later attempts |
Tip: Ask clinics for a full breakdown upfront—no surprises!
Success Rates: What Are Your Chances?
Success isn’t guaranteed with IVF, but the odds have gotten better. According to the CDC’s 2021 data (the latest detailed stats), about 50% of cycles for women under 35 lead to a live birth. That drops with age—around 20% for women 38-40, and 10% for those over 40 using their own eggs.
What boosts your chances?
✔️ Younger age (or donor eggs if you’re older).
✔️ Healthy lifestyle—think good diet and no smoking.
✔️ Top-notch clinics with high success rates.
What lowers them?
❌ Extra weight (over or under).
❌ Stress (it’s tricky to avoid, but it matters).
❌ Poor embryo quality.
Want to test your knowledge? Here’s a quick quiz:
Mini Quiz: What Affects IVF Success?
- Does age matter? (A) Yes (B) No
- Can smoking hurt your chances? (A) Yes (B) No
- Is every cycle a sure thing? (A) Yes (B) No
Answers: 1-A, 2-A, 3-B. How’d you do?
Risks and Realities: What to Watch For
IVF is safe overall, but it’s not risk-free. Here’s what might come up:
- Ovarian Hyperstimulation Syndrome (OHSS): The fertility drugs can overstimulate your ovaries, causing swelling and fluid buildup. It’s rare (1-5% of cases) and usually mild, but severe cases need a doctor’s care.
- Multiple Births: Transferring more than one embryo can lead to twins or triplets, which ups the risk of early delivery or complications.
- Emotional Toll: As we talked about, the ups and downs can wear you out.
A 2023 study from the Mayo Clinic found no link between IVF drugs and ovarian cancer—a big relief for many. Still, talk to your doctor about any worries.
IVF Around the World: A Global Snapshot
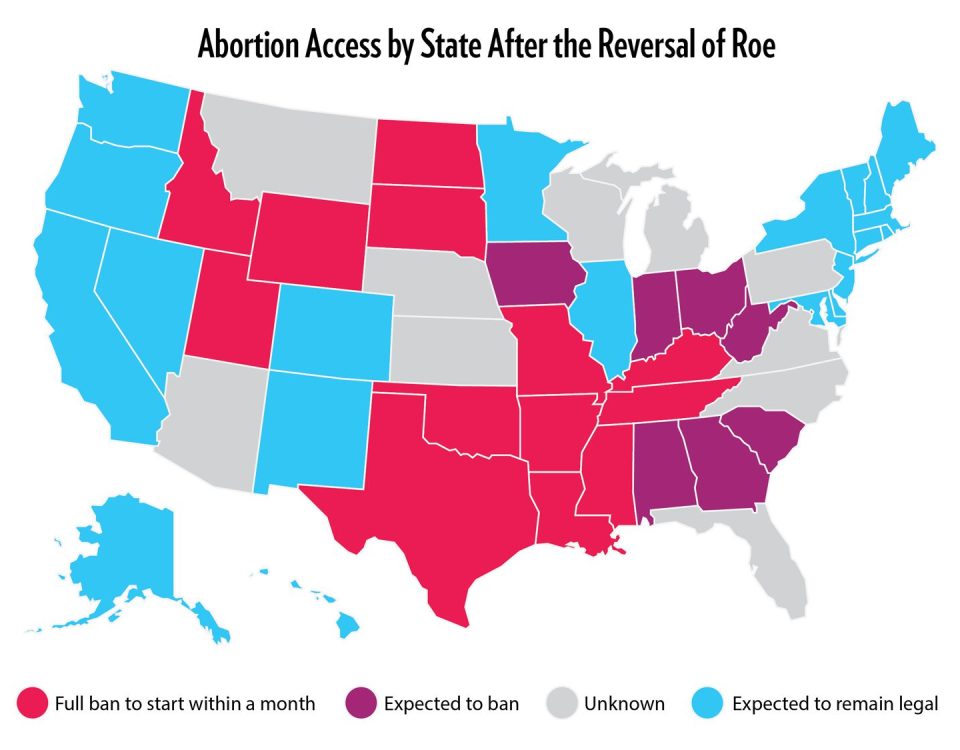
IVF isn’t the same everywhere. In the U.S., it’s pricey and often out-of-pocket. In places like Denmark or Israel, governments fund multiple cycles—sometimes up to three for free. Japan’s even jumping in, with 2023 plans to cover IVF through insurance to boost birth rates.
Why the difference? Culture, money, and laws play a role. Some countries limit who can use IVF (like barring single women), while others embrace it widely. It’s a reminder that where you live shapes your options.
Three Things You Haven’t Heard About IVF
Most articles stick to the basics, but here are some fresh angles:
1. The Microbiome Connection
Your gut health might affect IVF success. A 2024 study from Stanford suggested that a balanced microbiome (the bacteria in your body) could improve embryo implantation. They’re still figuring it out, but eating yogurt or probiotics might be a simple boost. No one’s talking about this yet—it’s brand new!
2. The “Quiet Embryo” Theory
Some researchers think the best embryos are the quiet ones—meaning they don’t use up tons of energy early on. A 2025 paper from the American Society for Reproductive Medicine found these low-metabolism embryos might implant better. It’s a shift from picking the flashiest ones and could change how labs choose.
3. Virtual Reality Support
Clinics are testing VR to ease IVF stress. Imagine slipping on goggles to “visit” a calm beach during a procedure. A small 2024 trial in Boston saw patients report 30% less anxiety with VR. It’s not widespread, but it’s a peek at how tech could help your mind, not just your body.
Your IVF Action Plan: Tips to Get Started
Ready to explore IVF? Here’s a practical guide to kick things off:
- Find a Clinic: Look for one with good reviews and high success rates. The CDC’s ART database is a goldmine for stats.
- Ask Questions: How many cycles do they recommend? What’s their approach to your specific issue?
- Prep Your Body: Eat well, sleep lots, and cut stress where you can. A 2023 study showed 8 hours of sleep nightly upped success by 10%.
- Budget Smart: Save up, check insurance, or apply for grants early.
- Build a Team: Line up a counselor or friend to lean on—support matters.
Poll Time! What’s your biggest IVF question?
A) Cost
B) Success rates
C) Emotional stuff
D) Something else
Drop your pick in your head—or share it with a friend!
The Future of IVF: What’s Next?
IVF’s not slowing down. By 2030, experts predict costs could drop thanks to automation—like that lab-on-a-chip idea. Genetic tools might get sharper, spotting tiny issues before transfer. And if IVG pans out, it could rewrite who can have biological kids.
For now, it’s about making it work for you. Whether you’re dreaming of a baby or just curious, IVF’s a mix of science, grit, and a little magic. It’s not perfect, but for millions, it’s been a game-changer.
So, what do you think? IVF’s a big topic, but it’s all about real people and real stories. Maybe it’s your story—or someone you love. Either way, it’s a window into how far we’ve come and where we’re going. Got thoughts? Share them with someone—it’s a conversation worth having!