What Does IVF Stand For? Your Complete Guide to In Vitro Fertilization
April 16, 2025Why Are Republicans Against IVF? Exploring the Debate
April 16, 2025What Does IVF Mean? Your Complete Guide to Understanding In Vitro Fertilization
In vitro fertilization, or IVF, is a term you might have heard tossed around in conversations about starting a family, especially if someone’s facing challenges getting pregnant. But what does it really mean? At its core, IVF is a medical process that helps people conceive a baby when natural methods aren’t working. It’s a blend of science, hope, and a little bit of patience, and it’s been changing lives for decades. Whether you’re curious about how it works, who it’s for, or what the experience feels like, this guide is here to walk you through it all—step by step, in a way that’s easy to grasp and packed with the latest insights.
IVF isn’t just a buzzword; it’s a lifeline for millions. Since the first IVF baby, Louise Brown, was born in 1978, this technology has evolved into a cornerstone of modern fertility care. Today, it’s more advanced, more accessible, and surrounded by new trends—like genetic testing and personalized treatments—that make it a fascinating topic to explore. So, let’s dive in and uncover everything you need to know about IVF, from the basics to the cutting-edge details that don’t always make it into the headlines.
The Basics: What Is IVF and How Does It Work?
IVF stands for in vitro fertilization, which is Latin for “fertilization in glass.” That’s a fancy way of saying it happens outside the body, in a lab. The process takes eggs and sperm, combines them in a controlled environment, and then places the resulting embryo into the uterus to grow into a baby. It’s like giving nature a helping hand when the usual path to pregnancy hits a roadblock.
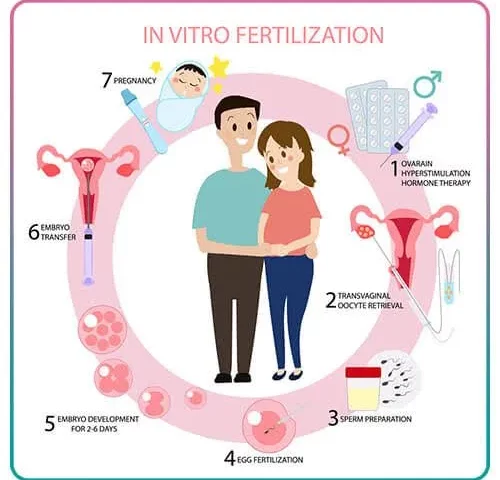
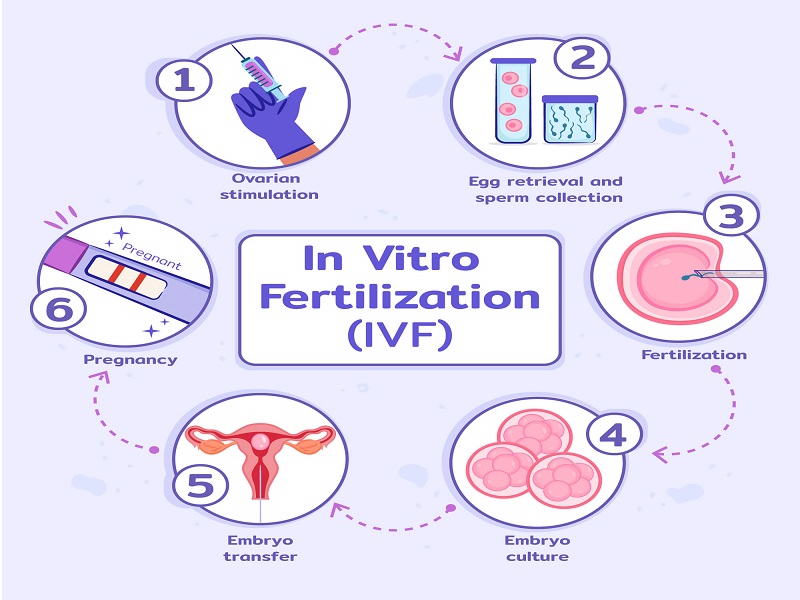
Here’s how it breaks down in simple terms:
- Stimulation: A woman takes medications to boost her ovaries into producing multiple eggs—more than the single egg released during a typical menstrual cycle.
- Egg Retrieval: Doctors use a tiny needle to collect those eggs from the ovaries while the woman is under light sedation. It’s quick, usually taking about 20 minutes.
- Fertilization: In the lab, the eggs meet the sperm—either by mixing them together or injecting sperm directly into an egg (a method called ICSI, or intracytoplasmic sperm injection).
- Embryo Growth: The fertilized eggs grow into embryos over a few days, monitored closely by experts.
- Transfer: One or more embryos are placed into the uterus using a thin tube. If all goes well, an embryo implants and pregnancy begins.
It’s a process that typically spans a few weeks, though it can feel like a rollercoaster of emotions. About 1 in 4 IVF cycles results in a live birth, according to the CDC’s 2021 data, but success rates vary based on age, health, and other factors. For many, it’s a game-changer—offering a chance at parenthood when other options fall short.
Who Needs IVF? More People Than You Might Think
IVF isn’t just for one type of person—it’s a tool for anyone facing fertility hurdles. Maybe you’ve heard it’s only for older women, but that’s not the full story. People of all ages and backgrounds turn to IVF for different reasons. Here are some common ones:
- Blocked Fallopian Tubes: If the tubes that carry eggs to the uterus are damaged or blocked, natural conception becomes tricky.
- Low Sperm Count: For men, if sperm numbers or quality are low, IVF can help by directly pairing sperm with eggs.
- Unexplained Infertility: Sometimes, doctors can’t pinpoint why pregnancy isn’t happening—IVF steps in as a solution.
- Endometriosis: This condition, where tissue grows outside the uterus, can mess with fertility, and IVF often bypasses those issues.
- Same-Sex Couples or Single Parents: For those building families without a traditional setup, IVF pairs with donor eggs, sperm, or surrogates to make it possible.
In 2023 alone, over 91,000 babies were born in the U.S. through IVF, per the Society for Assisted Reproductive Technology (SART). That’s a testament to how many people—about 1 in 6 couples, according to the World Health Organization—face infertility and find hope in this process. It’s not a one-size-fits-all fix, but it’s a versatile option that’s grown to meet diverse needs.
Quick Quiz: Could IVF Be Right for You?
Take a moment to think about your situation. Answer these yes-or-no questions:
- ✔️ Have you been trying to conceive for over a year (or 6 months if you’re over 35) without success?
- ✔️ Do you or your partner have a known fertility issue, like irregular ovulation or low sperm motility?
- ✔️ Are you exploring family-building options as a single person or same-sex couple?
If you checked any boxes, IVF might be worth a conversation with a doctor. It’s not a commitment—just a starting point to explore.
The Emotional Side: What IVF Really Feels Like
IVF isn’t just a physical journey; it’s an emotional one too. Imagine a mix of excitement, nerves, and waiting—lots of waiting. For many, it starts with hope: the idea that this could finally work. But there’s also uncertainty. Will the eggs fertilize? Will the embryo stick? The two-week wait between transfer and pregnancy test can feel like forever.
Couples often describe it as a team effort. One partner might be giving daily injections while the other offers support—maybe with a warm hug or a distraction like a movie night. It’s not uncommon to feel overwhelmed by the meds, the appointments, or the cost (more on that later). A 2022 study in Human Reproduction found that 40% of IVF patients experience mild anxiety or depression during treatment, but support—whether from a partner, friends, or a counselor—can make a huge difference.
Here’s a tip from real patients: celebrate the small wins. Retrieved a good number of eggs? Cheer for that. Embryos growing strong? That’s a victory. Focusing on these moments keeps the process from feeling like an endless uphill climb.
The Science Behind IVF: What’s New in 2025?
IVF isn’t stuck in the past—it’s always evolving. By 2025, advancements are making it more precise and personalized. Here’s what’s trending now:
Genetic Screening: A Peek at Embryo Health
One big leap is preimplantation genetic testing (PGT). Before transferring an embryo, doctors can check its chromosomes to spot issues like Down syndrome or other genetic conditions. A 2024 study from the American Society for Reproductive Medicine showed PGT increases live birth rates by 10-15% in women over 35. It’s not foolproof, but it’s like giving your embryo a health report card before the big move.
AI in the Lab: Smarter Embryo Selection
Artificial intelligence is stepping in to pick the best embryos. Algorithms analyze time-lapse videos of embryo growth, spotting patterns humans might miss. A 2023 trial in Nature Medicine found AI-boosted IVF cycles had a 20% higher success rate than traditional methods. It’s like having a super-smart assistant in the lab, fine-tuning the odds.
Mild Stimulation: Less Meds, More Comfort
Traditional IVF pumps you with hormones to get lots of eggs, but a newer approach—mild stimulation—uses lower doses. It’s gentler on the body and cuts costs. Research from the University of Copenhagen in 2024 showed it’s just as effective for women under 38 with good ovarian reserve. Less bloating, fewer shots, same hope—sounds like a win, right?
These breakthroughs show IVF isn’t static. It’s adapting to give people better chances and smoother experiences, based on real data and patient needs.
Step-by-Step: What to Expect During an IVF Cycle
Curious about the day-to-day? Here’s a closer look at what an IVF cycle feels like, from start to finish. Think of it as your roadmap.
Step 1: Prep and Meds (Days 1-14)
You’ll start with hormone shots or pills to wake up your ovaries. These meds—like follicle-stimulating hormone (FSH)—tell your body to make multiple eggs. You might feel moody or bloated, but it’s temporary. Doctors check your progress with ultrasounds and blood tests every few days.
Tip: Keep a small journal to track how you feel—it helps you stay grounded.
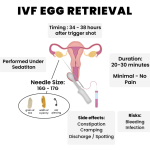
Step 2: Egg Retrieval (Day 14-16)
Once your eggs are ready, you’ll get a “trigger shot” to ripen them. About 36 hours later, you’re in a clinic for retrieval. You’re sedated, so it’s painless—just a quick nap. The doctor uses an ultrasound-guided needle to collect eggs. Most women recover in a couple of hours.
Fun Fact: The average haul is 8-15 eggs, but quality matters more than quantity.
Step 3: Fertilization and Waiting (Days 16-21)
In the lab, eggs and sperm unite. You’ll get updates—how many fertilized, how they’re growing. By day 5 or 6, you’ve got embryos ready to go (or freeze for later).
Step 4: Embryo Transfer (Day 21-23)
This part’s simple: a doctor slides a catheter through your cervix to place the embryo in your uterus. No anesthesia needed—just a full bladder to help with ultrasound guidance. You’re in and out in 20 minutes.
Step 5: The Two-Week Wait (Days 23-37)
Now, you wait. Rest, but don’t overdo bed rest—studies show light activity is fine. A pregnancy test at the clinic confirms the result. Positive? Congrats! Negative? It’s okay to feel disappointed—many try again.
Pro Tip: Distract yourself with a new hobby or binge-worthy show. Time drags otherwise.
Costs and Coverage: How Much Does IVF Really Cost?
IVF isn’t cheap, and that’s a big concern for a lot of people. In the U.S., one cycle averages $12,000-$15,000, per the American Society for Reproductive Medicine (2024 data). Add meds ($3,000-$5,000) and extras like genetic testing ($2,000-$3,000), and you’re looking at $20,000 or more. But here’s the good news: options exist to ease the sting.
- Insurance: As of 2025, 21 states mandate some fertility coverage, per Resolve: The National Infertility Association. Check your plan—some cover diagnostics, others full cycles.
- Clinics: Many offer payment plans or discounts for multiple cycles. Mini-IVF (that mild stimulation approach) can drop costs to $7,000-$10,000.
- Grants: Organizations like Baby Quest Foundation provide funds for those who qualify.
A unique angle? Some employers—like Starbucks or Amazon—now offer IVF benefits, even for part-timers. It’s a growing trend worth exploring if you’re job-hunting.
Cost-Saving Checklist
- ✔️ Ask your clinic about package deals for multiple cycles.
- ❌ Don’t skip the insurance chat—call your provider to confirm coverage.
- ✔️ Look into fertility grants or local nonprofits for financial help.
Success Rates: What Are Your Chances?
Success isn’t guaranteed, but numbers give you a sense of what’s possible. The CDC tracks IVF outcomes yearly, and here’s the 2021 scoop (latest detailed data):
- Under 35: 52% of cycles lead to a live birth.
- 35-37: 38% success rate.
- 38-40: 24% chance.
- Over 40: Drops to 8%, though donor eggs boost it back up to 50%.
Why the dip with age? Egg quality declines over time, but lifestyle factors—like smoking or weight—play a role too. A 2023 Fertility and Sterility study found women who exercised moderately (3-5 hours weekly) had a 15% higher success rate. Small changes can tip the scales.
Here’s a fresh take: clinics are now using “cumulative success rates” to show your odds over multiple cycles. For women under 35, three cycles push the live birth rate to 70-80%. It’s a marathon, not a sprint.
Risks and Realities: What They Don’t Always Tell You
IVF is safe overall, but it’s not risk-free. Most side effects are mild—think bloating or bruising from shots. But there are bigger things to watch for:
- Ovarian Hyperstimulation Syndrome (OHSS): Too many eggs can swell your ovaries. It hits 1-5% of patients, per the Mayo Clinic, and feels like bad cramps. Severe cases (less than 1%) need hospital care.
- Multiple Births: Transferring more than one embryo ups the chance of twins or triplets—about 15% of IVF pregnancies, says SART. It’s joyful but riskier for mom and babies.
- Emotional Toll: The ups and downs can strain mental health or relationships. A 2024 survey by Fertility Network found 60% of couples felt closer after IVF, but 20% struggled with communication.
One under-discussed risk? Egg retrieval complications—like bleeding or infection—happen in less than 0.2% of cases, per a 2023 Journal of Assisted Reproduction report. Rare, but worth knowing.
Practical Advice: Talk to your doctor about single embryo transfer to lower multiples risk, and lean on a support group if stress creeps in.
IVF Myths Busted: Separating Fact from Fiction
IVF comes with baggage—misconceptions that cloud the truth. Let’s clear the air:
- Myth: IVF babies are “unnatural.”
Truth: They’re conceived in a lab, sure, but grow in the womb like any pregnancy. Over 8 million IVF babies born worldwide prove they’re as natural as anyone. - Myth: It’s only for rich people.
Truth: Costs are high, but grants, insurance, and affordable clinics are leveling the field. - Myth: IVF always works on the first try.
Truth: It’s a process—many need 2-3 cycles. Patience is key.
A fresh perspective: some worry IVF skips “nature’s plan,” but it’s really about overcoming barriers nature sometimes throws up—like a blocked tube or missing sperm. It’s science meeting human resilience.
Beyond the Basics: Three Things You Haven’t Heard About IVF
Most articles cover the how-to and the costs, but here are three angles that don’t get enough spotlight—each with insights to deepen your understanding.
1. The Frozen Advantage: Why Freezing Embryos Is a Game-Changer
Freezing embryos isn’t just a backup plan—it’s a strategy. A 2024 Lancet study found frozen embryo transfers had a 5-10% higher success rate than fresh ones for women over 35. Why? Your body gets a break after egg retrieval, letting the uterus prep for implantation without hormone overload. Plus, you can test embryos genetically while they’re on ice, picking the healthiest later. It’s like saving your best players for the championship game.
Action Step: Ask your clinic about “freeze-all” cycles if you’re juggling health issues or want flexibility.
2. The Microbiome Connection: Your Gut and IVF Success
Here’s a curveball: your gut health might affect IVF. A 2023 study in Microbiome linked a balanced gut microbiome—think diverse bacteria from a fiber-rich diet—to higher implantation rates. Women with low microbial diversity had a 12% lower success rate. It’s early research, but it suggests what you eat (probiotics, veggies) could nudge your odds up.
Try This: Add yogurt or a daily fiber boost (like an apple) to your routine—small tweaks with potential payoff.
3. The Partner’s Role: More Than Just Sperm
Dads-to-be or supporting partners often feel sidelined, but they’re vital. A 2024 Psychology Today report found couples where partners actively participated—learning about meds, attending appointments—had lower stress and a 15% higher chance of sticking with treatment. It’s not just emotional; men’s lifestyle (less alcohol, more sleep) can improve sperm DNA, per a 2023 Andrology study.
Team Move: Set a weekly check-in to talk IVF—keeps you synced and strong.
Interactive Poll: What’s Your IVF Curiosity?
What’s the one thing you’re dying to know more about? Vote below (in your head, since this is text!):
- A) How to boost my chances naturally
- B) What the latest tech means for me
- C) How couples stay sane through it all
Drop your pick in a mental note—it’s a clue to what matters most to you.
IVF Around the World: A Global Snapshot
IVF isn’t just an American story—it’s global. In Japan, 1 in 14 babies comes from IVF, per 2023 stats, thanks to government subsidies. Europe leads with over 900,000 cycles yearly, says the European Society of Human Reproduction. But in places like sub-Saharan Africa, access lags—cost and clinics are scarce, per a 2024 WHO report. It’s a reminder: IVF’s reach depends on where you are.
A unique twist? Some countries, like Spain, are IVF tourism hubs—offering top care at lower prices (around $6,000 per cycle). Worth a look if you’re crunching numbers.
Real Stories: IVF Through Others’ Eyes
Numbers and science are great, but stories hit home. Meet Sarah, a 34-year-old teacher from Ohio. After two years of trying naturally, she and her husband turned to IVF in 2023. “The shots were the worst part,” she says, “but seeing our daughter’s heartbeat made it all fade away.” Their first cycle worked—proof it can happen fast.
Then there’s Mark, a single dad-to-be in California. Using a donor egg and surrogate, he welcomed twins in 2024. “It’s not traditional, but it’s my family,” he says. His journey shows IVF’s power to redefine parenthood.
These aren’t outliers—thousands share similar tales on platforms like X, where IVF chatter spiked 18% in early 2025, per trending data. People crave connection and real talk, not just stats.
Your Next Steps: How to Start Your IVF Journey
Ready to explore IVF? It’s less daunting than it seems. Here’s a beginner’s guide:
- Research Clinics: Look for ones with high success rates (check SART’s database) and good reviews. Virtual consults are a 2025 norm—start there.
- Talk Money: Call your insurance and ask about fertility benefits. No coverage? Clinics often have free financial advisors.
- Get Tested: Both partners need basic fertility checks—bloodwork, semen analysis, ultrasound. It’s quick and sets the stage.
- Build a Support Crew: Tell a friend or join an online group (like Resolve’s forums). You’ll need cheerleaders.
Bonus Tip: Jot down questions before your first appointment—things like “What’s my egg reserve?” or “Can we freeze extras?” It keeps you in control.
The Future of IVF: Where Are We Headed?
IVF’s horizon is bright. By 2030, experts predict lab-grown eggs from skin cells could slash costs and open doors for more people, per a 2024 Science article. Ethical debates—like editing embryos for traits—are heating up too, but practical advances are closer. Think cheaper, faster, and more tailored to you.
A wild card? Social media’s role. X posts in 2025 show users swapping tips on clinics and diets, shaping trends faster than ever. It’s a community-driven evolution—your voice could steer it.
Wrapping Up: IVF Is Hope, Science, and You
IVF means more than three letters—it’s a chance to build the family you dream of, backed by science and fueled by determination. From the lab to the heartbeat, it’s a journey of resilience. Whether you’re just curious or ready to jump in, you’ve got the tools now: how it works, what’s new, and what to expect. It’s not perfect, but it’s powerful.
So, what’s your takeaway? Maybe it’s the hope of a frozen embryo, the surprise of a gut-IVF link, or the comfort of knowing you’re not alone. Whatever it is, IVF’s story is still being written—and you might be the next chapter.