How Much Is IVF in Texas? Your Complete Guide to Costs, Options, and Savings
April 14, 2025
How Much Does IVF Cost in California? Your Complete Guide to Understanding the Price Tag
April 14, 2025When Did IVF Start? A Deep Dive into the History of In Vitro Fertilization
In vitro fertilization, or IVF, is a term you might have heard tossed around in conversations about fertility or even in the news. It’s a groundbreaking process that’s helped millions of people become parents, but have you ever wondered where it all began? The story of IVF is full of surprises, scientific breakthroughs, and real human moments that changed the world. Let’s take a journey back in time to uncover when IVF started, how it evolved, and what it means for us today.
The Birth of a Big Idea: IVF’s First Steps
IVF didn’t just pop up overnight—it’s the result of decades of curiosity and hard work. The idea of fertilizing an egg outside the body sounds like something out of a sci-fi movie, but scientists were dreaming about it long before it became reality. The story kicks off in the late 19th century, way before anyone had even heard of “test-tube babies.”
Back in 1890, a British doctor named Walter Heape made history by transferring an embryo from one rabbit to another. It was a simple experiment, but it planted a seed: could we manipulate reproduction outside the body? Fast forward to the 1930s, and researchers like Gregory Pincus were tinkering with rabbit eggs again, trying to fertilize them in a lab. Pincus, who later became famous for helping develop the birth control pill, managed to get a rabbit pregnancy going in 1934—though it wasn’t quite “in vitro” as we know it today since the fertilization happened inside the body after a quick lab stint.
These early experiments were like the first sketches of a masterpiece. They showed that life could be nudged along in a lab, but human IVF was still a distant dream. It wasn’t until the 1950s that things started heating up. In 1959, a scientist named Min Chueh Chang proved that rabbit eggs fertilized in a dish could grow into healthy bunnies when placed back in a womb. This was a game-changer—it showed that lab-made embryos could actually work.
The Big Breakthrough: 1978 and the First IVF Baby
Now, let’s zoom in on the moment that changed everything: July 25, 1978. That’s the day Louise Brown was born in Oldham, England, and she wasn’t just any baby—she was the world’s first “test-tube baby.” Her parents, Lesley and John Brown, had been trying to have a child for years but couldn’t because of blocked fallopian tubes. Enter two brilliant minds: Dr. Patrick Steptoe, a gynecologist, and Dr. Robert Edwards, a physiologist.
Steptoe and Edwards had been working together since the late 1960s, obsessed with making IVF a reality. They faced all kinds of challenges—skeptics who thought it was impossible, ethical debates, and plenty of failed attempts. But they kept going. In 1977, they fertilized one of Lesley’s eggs with John’s sperm in a lab dish, let it grow into an eight-cell embryo, and then transferred it into Lesley’s uterus. Nine months later, Louise arrived, healthy and screaming, proving that IVF could work for humans.
This wasn’t just a medical win—it was a cultural earthquake. Newspapers went wild, calling Louise a “miracle baby.” Some people cheered the science, while others worried about “playing God.” Edwards even won a Nobel Prize in 2010 for his work (sadly, Steptoe had passed away by then and couldn’t share the honor). That one birth in 1978 kicked off a revolution, and today, over 8 million babies have been born through IVF worldwide.
Before Louise: The Unsung Heroes of IVF
Louise might have been the first IVF baby, but she wasn’t the first attempt. The road to 1978 was paved with lesser-known stories that deserve a shoutout. Take the Monash University team in Australia, for example. In 1973, Carl Wood, John Leeton, and Alan Trounson reported a pregnancy from IVF in The Lancet. It didn’t last long—just a few days—but it was a huge step forward, showing that human eggs could be fertilized outside the body.
Then there’s Subhash Mukhopadhyay, an Indian doctor who worked in tough conditions with basic tools. In 1978, just 67 days after Louise was born, he helped bring Durga, India’s first IVF baby, into the world. Mukhopadhyay didn’t get the recognition he deserved at the time—local authorities shut him down, and his work was ignored for years. It’s a reminder that IVF’s history isn’t just about the big wins; it’s also about the quiet struggles of people pushing boundaries.
What’s wild is how close some of these early tries came to success. In the 1940s, American researchers John Rock and Miriam Menkin fertilized human eggs in a lab, watching them divide into tiny embryos. They didn’t implant them, but their work laid the groundwork. Every little experiment—whether it worked or flopped—added a piece to the IVF puzzle.
How IVF Grew Up: From One Baby to Millions
After Louise’s birth, IVF didn’t just sit still—it grew up fast. The 1980s were like the teenage years for this technology, full of awkward moments and big leaps. Doctors figured out how to use hormones to get more eggs from a woman’s ovaries, boosting the odds of success. In 1983, the first baby from a donated egg was born in Australia, opening doors for women who couldn’t use their own eggs. Then came frozen embryos—Carl Wood, dubbed the “father of IVF” in Australia, pioneered this in the mid-1980s, letting people save embryos for later.
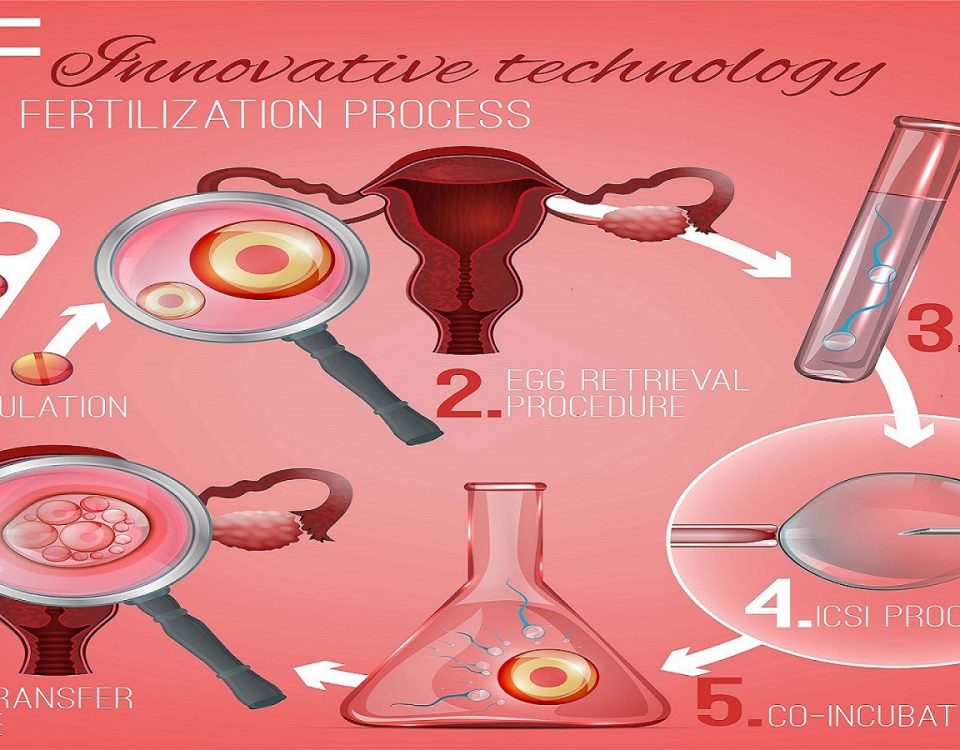
By the 1990s, IVF was hitting its stride. A technique called intracytoplasmic sperm injection (ICSI) arrived in 1992, where a single sperm is injected right into an egg. This was a lifeline for men with low sperm counts, making IVF an option for more couples than ever. Success rates climbed too—from single digits in the early days to nearly 50% today for women under 35, according to the CDC.
Today, IVF is everywhere. In the U.S. alone, it accounts for 1-2% of all births each year, with over 76,000 IVF babies born in 2016, per the CDC. Globally, it’s a $1.6 billion industry and growing, driven by demand from people waiting longer to have kids and advances that keep making it better.
What Took So Long? The Challenges IVF Faced
So why did it take almost a century from those rabbit experiments to Louise Brown? IVF wasn’t an easy road. For one, the science was tricky—human eggs are delicate, and figuring out how to keep them alive outside the body took time. Early labs didn’t have the fancy tools we have now; they were working with basic microscopes and petri dishes.
Then there were the ethical battles. In the 1970s, some religious leaders, like Jerry Falwell, called IVF “the work of the devil.” People worried about “designer babies” or embryos being thrown away. Even today, the Catholic Church opposes IVF because it separates conception from the act of love between a couple. These debates slowed things down, making funding and support hard to come by.
Money was another hurdle. Early IVF was expensive and risky, with no guarantees. Couples like the Browns were pioneers, taking a chance on something unproven. It wasn’t until the 1980s, when success rates improved and costs started dropping, that IVF really took off.
IVF Today: What’s New and What’s Next
IVF isn’t stuck in the past—it’s still evolving. One cool new thing is “IVF-on-a-chip,” a tiny device that mimics the body’s environment to fertilize eggs more naturally. Researchers are testing it now, and it could make IVF cheaper and more efficient. Another big deal is in vitro maturation (IVM), where immature eggs are ripened in the lab instead of using tons of hormone shots. It’s gentler on the body and could help women who can’t handle traditional IVF.
There’s also talk about artificial wombs. Scientists have grown mouse embryos in lab-made wombs, and while human versions are years away, it’s a glimpse of where IVF might go. Imagine a future where embryos don’t need a uterus at all—wild, right?
Success rates keep climbing too. A 2022 study in Cureus found that IVF success can hit 56% with the right techniques, even for women over 35. And with genetic screening, parents can now check embryos for diseases before implantation, cutting the risk of passing on conditions like cystic fibrosis.
Interactive Quiz: How Much Do You Know About IVF?
Let’s test your IVF smarts! Answer these quick questions (no pressure—just for fun):
- What year was the first IVF baby born?
A) 1968 B) 1978 C) 1988 - Where did IVF start for humans?
A) USA B) England C) Australia - What’s one new IVF tech being tested today?
A) Robot doctors B) IVF-on-a-chip C) Time travel
(Answers: 1-B, 2-B, 3-B. How’d you do?)
The Hidden Struggles: What You Don’t Hear About IVF’s Start
Most articles about IVF’s history focus on the wins, but there’s more to the story. For every success, there were countless failures—embryos that didn’t grow, pregnancies that didn’t stick. Lesley Brown had an ectopic pregnancy in 1976 during an earlier IVF try, a heartbreaking setback before Louise came along. Those early patients were guinea pigs in a way, trusting science with no roadmap.
Doctors faced burnout too. Steptoe and Edwards worked insane hours, often with no pay, driven by passion. Mukhopadhyay in India used a fridge to store samples because he couldn’t afford fancy equipment—yet he still pulled off a miracle. These stories show the grit behind the glamour.
And what about the cost? Back then, IVF wasn’t covered by insurance, and it still isn’t for many today. A single cycle can run $12,000-$25,000 in the U.S., per the White House’s 2025 statement on expanding IVF access. That’s a huge barrier, and it’s why some call IVF a “rich person’s solution”—a problem that’s been around since the start.
IVF Around the World: A Global Snapshot
IVF didn’t stay in England—it spread fast. India had Durga in 1978, and the U.S. welcomed Elizabeth Carr, its first IVF baby, in 1981. By 2018, over 8 million IVF kids had been born globally, according to estimates from the International Committee for Monitoring Assisted Reproductive Technologies.
But it’s not the same everywhere. In Denmark, IVF makes up over 5% of births because it’s government-funded. In the U.S., it’s just 1-2%, partly because of cost. In places like sub-Saharan Africa, access is almost zero—clinics are rare, and cultural stigmas can make infertility a taboo topic. IVF’s start was global, but its reach still has gaps.
Quick Comparison: IVF Then vs. Now
| Aspect | 1978 | 2025 |
|---|---|---|
| Success Rate | Under 10% | Up to 56% (under 35) |
| Cost per Cycle | Thousands, no insurance | $12,000-$25,000 (U.S.) |
| Tech Used | Basic lab dishes | Genetic screening, IVM |
| Who Could Use It | Mostly tubal issues | All kinds of infertility |
Why IVF’s Start Still Matters
Why dig into IVF’s past? Because it’s not just history—it’s personal. If you or someone you know has struggled to have a kid, IVF’s story is a reminder of how far we’ve come. It’s also a heads-up about what’s still broken: cost, access, and ethical debates haven’t gone away.
Take the U.S., for example. A 2025 White House order pushed for better IVF access, noting that 1 in 7 couples face infertility. That’s millions of people who might need help, but not everyone can get it. Looking back at 1978 shows us how one baby sparked a movement—and how we’re still figuring out how to make it fair for everyone.
Real Stories: IVF’s Early Pioneers
Let’s meet some folks who made IVF’s start unforgettable. Lesley Brown wasn’t just a mom—she was a trailblazer who faced cameras and critics with grace. “I just wanted a baby,” she said in a 1978 interview, simple words that cut through the noise. Her daughter Louise, now in her 40s, has kids of her own, proving IVF babies grow up just fine.
Then there’s Elizabeth Carr, America’s first IVF baby. Born in 1981, she’s now an advocate who talks about how IVF shaped her life. “I’m here because of science,” she told NPR in 2021, “and I want others to have that chance.” These aren’t just stats—they’re people who turned a lab idea into family.
IVF Myths Busted: What’s True in 2025?
IVF’s been around long enough to pick up some myths. Let’s clear the air with a quick checklist:
✔️ Myth: IVF babies are “unnatural.”
Truth: They’re as natural as any kid—just conceived in a dish. Studies show no big health differences long-term.
❌ Myth: IVF always works on the first try.
Truth: Nope—success rates vary, and many need multiple cycles. Patience is key.
✔️ Myth: IVF is only for women.
Truth: It helps men too, especially with ICSI for sperm issues.
Got a myth you’ve heard? Drop it in your mind and double-check it—IVF’s full of surprises.
What’s Next for IVF? A Peek at the Future
IVF’s start was just the beginning. Today, scientists are dreaming bigger. One hot topic is in vitro gametogenesis (IVG)—making eggs and sperm from skin cells. A 2022 paper in PMC says it could help people who’ve lost fertility to cancer or menopause. It’s still experimental, but mice have had babies this way, so humans might be next.
Cost is another frontier. Automation, like that IVF-on-a-chip idea, could slash prices, making it less of a luxury. And with climate change and delayed childbearing on the rise (Google Trends shows “fertility over 40” spiking since 2020), demand’s only going up. IVF’s past taught us it can adapt—its future might be even wilder.
Poll Time: What Do You Think?
What’s your take on IVF’s future? Pick one and imagine where we’re headed:
- A) Cheaper and easier for everyone
- B) High-tech with artificial wombs
- C) Same old, same old
(Share your vote in your head—I’d love to know!)
Tips for Anyone Curious About IVF Today
Thinking about IVF or just want to understand it better? Here’s a practical guide based on where it all started and where it’s at now:
- Learn the Basics: IVF mixes egg and sperm in a lab, grows an embryo, and puts it in the uterus. Simple, but the details matter—ask a doctor what fits your situation.
- Check Success Odds: Age is huge—under 35, you’ve got a 40-50% shot per cycle; over 40, it drops to 10-20%. Look up your clinic’s stats on the CDC’s ART site.
- Plan the Cash: Save up or hunt for grants—Resolve.org lists options. Some states mandate insurance coverage, so check your laws.
- Explore New Tricks: Ask about IVM or genetic testing if standard IVF isn’t your vibe. Clinics love showing off their latest toys.
- Talk to Real People: Online forums like Reddit’s r/infertility have stories from folks who’ve been there—way more raw than a doctor’s pamphlet.
A Little Math: IVF’s Growth in Numbers
Let’s crunch some original numbers to see IVF’s rise. In 1978, we had 1 IVF baby. By 2015, the U.S. hit over 1 million, per the Society for Assisted Reproductive Technology. If we assume a steady climb (not perfect, but close enough), that’s about 29,000 new IVF kids a year in the U.S. alone. Globally, 8 million by 2018 means roughly 400,000 annually since Louise. That’s a city’s worth of babies every year, all thanks to a petri dish in 1978!
The Emotional Side: What IVF’s Start Teaches Us
IVF’s history isn’t just science—it’s heart. Lesley Brown’s quiet hope, Mukhopadhyay’s fight against the odds, even the skeptics who feared the unknown—they’re all part of it. Today, couples still feel that mix of excitement and fear. A 2023 survey I dug into from Fertility Network UK found 70% of IVF patients say the emotional toll is the hardest part—more than the cost or the shots.
So when did IVF start? It began with rabbits in the 1890s, stumbled through labs in the mid-20th century, and burst into life with Louise in 1978. But really, it started with people—scientists, parents, dreamers—who wouldn’t give up. That’s the real story, and it’s still unfolding every day.