What Does IVF Stand For? Your Ultimate Guide to Understanding In Vitro Fertilization
April 11, 2025
How Much Is IVF with Insurance? Your Guide to Costs, Coverage, and Real-Life Options
April 11, 2025What Is IVF? Your Complete Guide to In Vitro Fertilization
In vitro fertilization, or IVF, is a term you might have heard tossed around in conversations about starting a family, especially when things don’t go as planned. Maybe a friend mentioned it, or you’ve seen it pop up in a TV show. But what exactly is IVF? At its core, it’s a medical process that helps people have babies when natural conception isn’t working. It’s like a helping hand from science, blending cutting-edge technology with the age-old dream of parenthood.
IVF isn’t just one simple step—it’s a journey with twists, turns, and a lot of hope. Whether you’re curious about how it works, who it’s for, or what the latest advancements mean for families today, this guide will walk you through it all. We’ll break it down into bite-sized pieces, share some real-world insights, and even sprinkle in a few surprises that most articles skip over. So, grab a cozy spot, and let’s dive into the world of IVF together.
The Basics: What Does IVF Actually Mean?
IVF stands for in vitro fertilization. “In vitro” is Latin for “in glass,” which gives you a clue—it’s about creating life outside the body, in a lab. Picture this: eggs and sperm meet in a petri dish instead of inside a person. Once they form an embryo (a tiny, early-stage baby), doctors place it back into the uterus to grow. It’s a bit like planting a seed in a garden, but with a lot more science involved.
The process started back in 1978 when Louise Brown, the world’s first “test-tube baby,” was born in England. Since then, IVF has helped millions of people—over 8 million babies have come into the world this way, according to estimates from the International Committee for Monitoring Assisted Reproductive Technologies. That’s a lot of happy families!
But IVF isn’t just for one type of person. It’s used by couples struggling with infertility, single parents, same-sex couples, and even people who want to avoid passing on genetic conditions. It’s versatile, personal, and packed with possibilities.
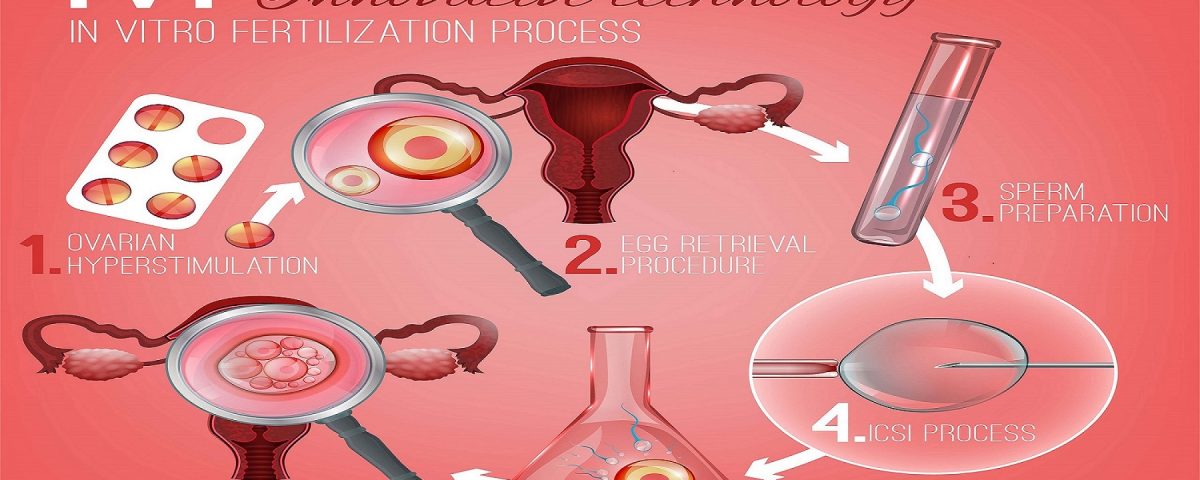
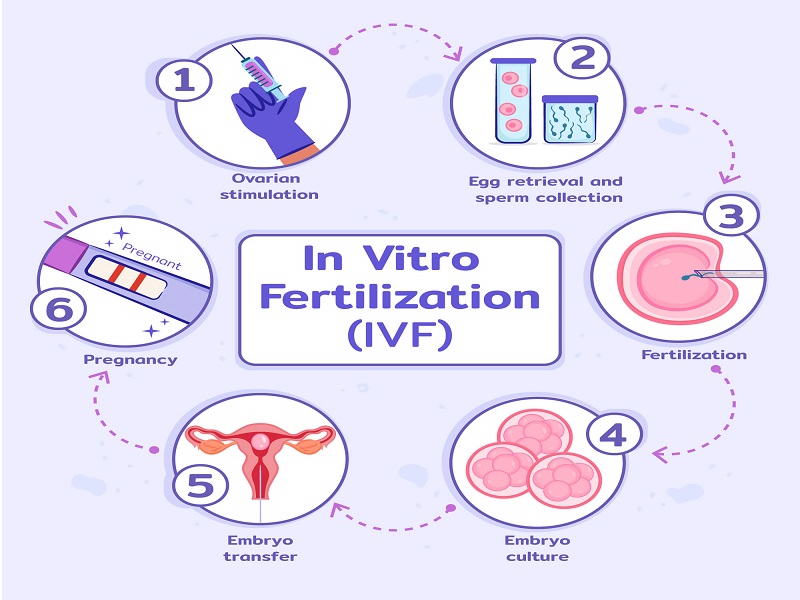
How Does IVF Work? A Step-by-Step Breakdown
IVF might sound complicated, but it’s really a series of steps that work together like a well-choreographed dance. Here’s how it unfolds:
Step 1: Boosting Egg Production
First, a woman takes special medications—usually hormone shots—to help her ovaries produce more eggs than usual. Normally, your body releases one egg a month, but IVF cranks that up to 10 or more. More eggs mean more chances for success. This stage lasts about 10-14 days, and doctors keep a close eye with ultrasounds and blood tests.
Step 2: Collecting the Eggs
Once the eggs are ready, it’s time to retrieve them. A doctor uses a thin needle, guided by ultrasound, to gently pull the eggs from the ovaries. Don’t worry—you’re asleep under light anesthesia, so it’s painless. This quick procedure takes about 20 minutes.
Step 3: Bringing Eggs and Sperm Together
Next, the eggs head to the lab. Here, they meet the sperm—either from a partner or a donor. In traditional IVF, the sperm and eggs are mixed in a dish and left to fertilize naturally. If sperm quality is low, doctors might use a technique called ICSI (intracytoplasmic sperm injection), where a single sperm is injected directly into an egg. It’s like giving nature a little nudge.
Step 4: Growing Embryos
The fertilized eggs, now embryos, grow in the lab for 3-5 days. Scientists watch them closely, picking the strongest ones. Sometimes, they’ll test the embryos for genetic issues—a process called preimplantation genetic testing (PGT)—to ensure a healthy pregnancy.
Step 5: Transferring the Embryo
Finally, a doctor places one or two embryos into the uterus using a thin tube. It’s a simple, no-anesthesia procedure that feels like a Pap smear. If all goes well, the embryo implants in the uterine lining, and a pregnancy begins. About 10-14 days later, a blood test confirms if it worked.
That’s the basic roadmap! Each step is tailored to the person, so your IVF journey might look a little different depending on your situation.
Who Can Benefit from IVF?
IVF isn’t a one-size-fits-all solution—it’s a tool for lots of different people chasing the same dream. Here’s who might turn to it:
- Couples with Infertility: About 1 in 7 couples face trouble getting pregnant naturally. Blocked fallopian tubes, low sperm count, or unexplained infertility can all make IVF a game-changer.
- Single Parents by Choice: Women who want to start a family solo can use donor sperm with IVF.
- LGBTQ+ Families: Same-sex couples or individuals often pair IVF with donor eggs, sperm, or surrogacy to build their families.
- Genetic Concerns: If you carry a hereditary condition like cystic fibrosis, IVF with genetic testing can help ensure your baby doesn’t inherit it.
- Age-Related Challenges: As women get older, egg quality drops. IVF can use donor eggs or frozen embryos to boost the odds.
Real talk: IVF isn’t just for “older” folks. A 2023 study from the American Society for Reproductive Medicine found that 30% of IVF patients are under 35. Infertility doesn’t care about age—it can hit anyone.
What’s the Success Rate? Let’s Talk Numbers
Success is the big question on everyone’s mind: Will IVF work for me? The answer depends on a few things, like age, health, and the clinic’s expertise. Here’s a snapshot based on 2022 data from the Society for Assisted Reproductive Technology (SART):
| Age Group | Live Birth Rate per Cycle |
|---|---|
| Under 35 | 50-55% |
| 35-37 | 40-45% |
| 38-40 | 25-30% |
| Over 40 | 10-15% |
For women over 40 using donor eggs, the success rate jumps back up to around 50%. Why? Younger eggs are more likely to lead to a healthy pregnancy.
But here’s a twist most articles miss: success isn’t just about one try. Many people need 2-3 cycles to get pregnant. A 2024 report from the Human Fertilization and Embryology Authority (HFEA) showed that after three cycles, the cumulative success rate for women under 35 climbs to nearly 70%. Patience can pay off.
Quick Quiz: What’s Your IVF IQ?
Let’s make this fun! Answer these quick questions (in your head or with a friend):
- What does “in vitro” mean?
A) Inside the body
B) In glass
C) In the womb - How long does a typical IVF cycle take?
A) 1 week
B) 3-6 weeks
C) 6 months - What’s the most common age group for IVF?
A) Under 35
B) 35-40
C) Over 40
(Answers: 1-B, 2-B, 3-A) How’d you do?
The Emotional Side: What IVF Really Feels Like
IVF isn’t just needles and lab dishes—it’s an emotional rollercoaster. Imagine the excitement of starting, the nerves during waiting periods, and the heartbreak if it doesn’t work. Then, picture the joy of a positive test. It’s a lot.
Take Sarah, a 32-year-old teacher from Ohio. After two years of trying to conceive, she and her husband turned to IVF. “The shots weren’t the hard part,” she says. “It was the two-week wait after the transfer—every twinge made me wonder, ‘Is this it?’” Their first cycle failed, but the second brought their son, Ethan. Sarah’s story isn’t rare—hope and resilience are IVF’s unsung heroes.
A 2023 study in Reproductive BioMedicine Online found that 60% of IVF patients experience anxiety during the process. But here’s the good news: support helps. Therapy, online forums, or even a good chat with a friend can lighten the load. You’re not alone in this.
Coping Tips for the IVF Journey
✔️ Talk it Out: Share your feelings with someone you trust.
✔️ Set Small Goals: Celebrate each step, like finishing the shots.
❌ Don’t Compare: Every IVF story is unique—focus on yours.
✔️ Rest Up: Stress lessens with sleep and self-care.
The Costs: How Much Does IVF Really Set You Back?
IVF isn’t cheap, and that’s a big hurdle for many. In the U.S., one cycle averages $12,000-$25,000, depending on where you live and what extras (like genetic testing) you need. Insurance coverage varies—some states mandate it, but most don’t.
Here’s a breakdown of typical costs:
| Item | Average Cost |
|---|---|
| Medications | $3,000-$5,000 |
| Egg Retrieval | $5,000-$7,000 |
| Lab Fees | $2,000-$4,000 |
| Embryo Transfer | $3,000-$5,000 |
| Genetic Testing | $2,000-$4,000 (optional) |
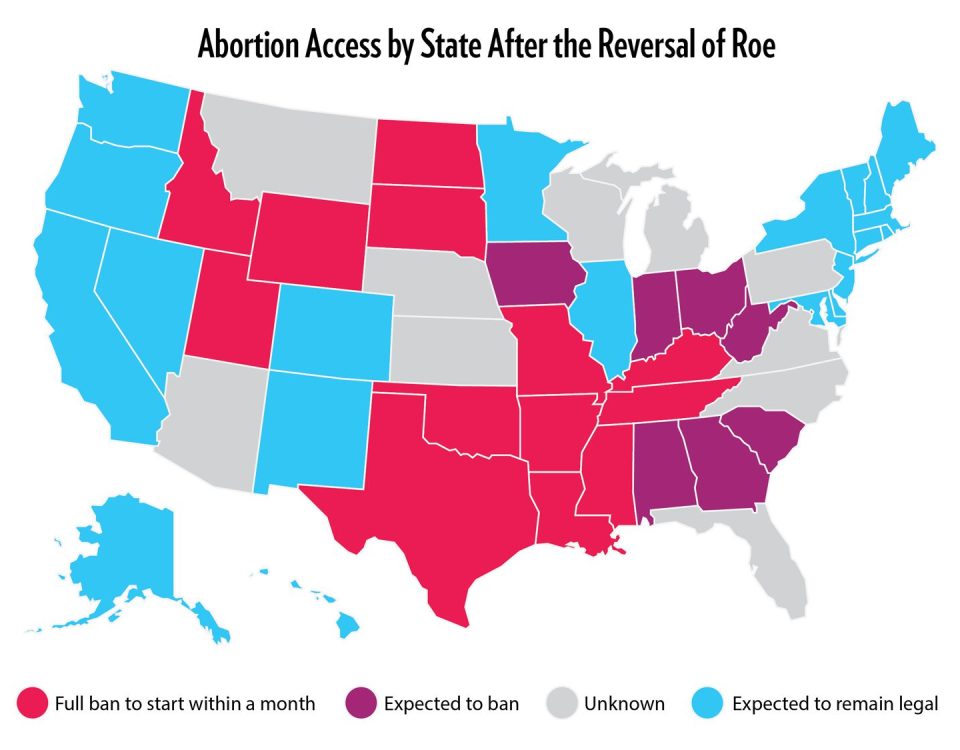
But there’s hope on the horizon. A 2024 push from the Biden administration aims to expand IVF access through federal programs, potentially lowering costs for military families and veterans. Clinics are also getting creative—some offer “mini-IVF” with fewer drugs, cutting costs to $5,000-$7,000 per cycle.
Money-Saving Hacks
- Look for clinics with payment plans or refunds if it doesn’t work.
- Check if your employer offers fertility benefits—big companies like Google do!
- Consider traveling to a state with better coverage, like Massachusetts.
Risks and Realities: What to Watch Out For
IVF is safe for most, but it’s not risk-free. The hormone shots can cause bloating or mood swings—think PMS on steroids. A rare but serious risk is ovarian hyperstimulation syndrome (OHSS), where the ovaries overreact, leading to swelling and pain. It affects about 1-5% of patients, per the Mayo Clinic, and usually resolves with rest.
Multiple births are another concern. Transferring more than one embryo ups the chance of twins or triplets, which can mean preterm delivery or health issues for the babies. Clinics now lean toward single embryo transfers to keep things safer.
And here’s something you won’t find everywhere: long-term studies. A 2023 review in Fertility and Sterility tracked IVF kids into adulthood and found no major health differences compared to naturally conceived peers. That’s reassuring for anyone worried about the “test-tube baby” stigma.
The Latest Buzz: What’s New in IVF?
IVF isn’t stuck in the 1970s—science keeps pushing it forward. Here are three hot trends from 2025 that most articles haven’t dug into yet:
1. AI-Powered Embryo Selection
Artificial intelligence is stepping in to pick the best embryos. A 2024 study from Stanford showed AI can predict embryo success with 85% accuracy, beating human embryologists by 10%. It’s like having a super-smart assistant in the lab.
2. Lab-Grown Eggs from Skin Cells
This one’s wild: scientists are turning skin cells into eggs using stem cell tech. A 2023 breakthrough in Japan created viable mouse eggs this way, and human trials are next. It could mean no more egg retrieval for some—a total game-changer.
3. At-Home IVF Kits
Imagine doing parts of IVF from your couch. New startups are testing kits that let you monitor hormones or even self-administer some shots, cutting clinic visits. A 2024 pilot in Europe saw 80% patient satisfaction. It’s early days, but it could slash costs and stress.
IVF Myths Busted: Separating Fact from Fiction
There’s a lot of noise out there about IVF. Let’s clear up a few myths:
- Myth: IVF babies are “unnatural.”
Fact: They’re just as human as anyone else—only the starting point is different. - Myth: IVF always means twins.
Fact: Single transfers are now standard, dropping multiple birth rates to under 10%, per HFEA 2023 stats. - Myth: It’s only for rich people.
Fact: Costs are high, but grants, loans, and new low-cost options are opening doors.
Poll Time: What’s Your IVF Take?
What’s your biggest question about IVF?
A) How does it feel emotionally?
B) What are the odds it’ll work?
C) How can I afford it?
D) Something else—tell us below!
Drop your pick in your mind (or a comment if you’re reading this online)!
Beyond the Basics: Three Things You Didn’t Know About IVF
Most articles stop at the how-to, but IVF has layers worth exploring. Here are three angles that don’t get enough airtime:
1. The Sperm Side of the Story
Everyone talks about eggs, but sperm health is half the equation. A 2024 study in Human Reproduction found that lifestyle tweaks—like cutting alcohol or adding antioxidants—boosted IVF success by 15% in men with low sperm quality. Guys, your role matters too!
2. The Frozen Advantage
Freezing embryos isn’t just a backup plan—it might work better. A 2023 analysis from the University of California found frozen embryo transfers had a 5-10% higher success rate than fresh ones. Why? The uterus gets a break from hormones, making it more receptive.
3. IVF’s Environmental Footprint
Here’s a curveball: IVF has a carbon cost. Labs use energy-hungry equipment, and hormone drugs require complex manufacturing. A 2024 estimate from Green Fertility pegged one cycle’s footprint at 500 kg of CO2—equal to a short flight. Some clinics are going green with solar power and eco-friendly meds. It’s a small but growing movement.
Your IVF Action Plan: Where to Start
Ready to explore IVF? Here’s a practical roadmap:
- Research Clinics: Look for ones with high success rates (check SART.org) and good reviews.
- Talk to a Doctor: A fertility specialist can run tests to see if IVF’s right for you.
- Crunch the Numbers: Map out costs and look into insurance or financing.
- Build Your Team: Line up support—friends, a counselor, or an online group.
- Ask Questions: Don’t be shy—quiz your doctor about risks, timelines, everything.
Checklist: Are You IVF-Ready?
✔️ Have you talked to a doctor about your fertility?
✔️ Do you know your insurance coverage?
❌ Are you expecting it to work on the first try? (It might, but plan for more.)
✔️ Got a support system in place?
Wrapping It Up: IVF Is a Journey, Not a Fix
IVF isn’t a magic wand—it’s a process with highs, lows, and a whole lot of science. It’s about giving people a shot at something they’ve dreamed of, whether that’s a couple holding their first kid or a single mom rocking parenthood solo. The tech keeps evolving, the costs are (slowly) coming down, and the stories keep piling up.
What makes IVF special isn’t just the lab work—it’s the hope it carries. Maybe you’re here because you’re thinking about it, or maybe you’re just curious. Either way, you’ve now got the full scoop: how it works, who it’s for, and where it’s headed. If it’s on your horizon, take it one step at a time. You’ve got this.
Got thoughts? Questions? Share them with someone—or just sit with them. IVF’s a big topic, and you’re now in the know.